Cell Based Therapies for Asthma, Thesis Paper Example
Abstract
Asthma is a critical health condition that has claimed the lives of millions of people over the past decade. The condition is characterized by airway inflammation that moves from one stage to another if not treated immediately. The extent to which this condition affects the quality of life and overall well-being is remarkably great. It leads to profound physical functioning leading to early deaths among patients who suffer from it. Treatment of asthma has always been a major challenge in the medical field. The most common treatment of the condition is the administration of corticosteroids. However, this treatment comes with adverse impacts that can be very dangerous if used for a long time by asthma patients. Past studies have shown that corticosteroids cause damage to the extracellular matrix elements. In response to this challenge, new treatment options are slowly and steadily emerging including the utilization of cell therapies which currently seem quite promising. This section of the study seeks to examine different literature findings on the emerging cell therapies and how effective they are in the treatment and management of asthma. Some of the cell therapy advancements that this study focuses on include extracellular vesicles, MSCs, and immune cells. The findings indicate that the application of these cell therapies is on the rise. It is also shown that cell therapies are crucial in addressing challenges related to asthma. It suggests that enhancing the state of health and well-being among asthma patients should involve the intervention of appropriate cell therapies.
Literature Review: Cell-Based Therapies for Asthma
Introduction
Healthcare remains one of the most critical aspects of an economy. Countries and societies that seek to prosper and sustain their generations invest highly in healthcare. As explained by Yu et al. (2020), the health of a nation is a very fundamental pillar for the realization of the nation’s vision. How diseases are managed is one of the strongholds for maintaining a healthy nation. Conducting extensive research and understanding how to prevent or treat various diseases has continued to help improve the state of health of people and communities across the globe for centuries. Evidence suggests cancer, asthma, heart diseases, and diabetes are the leading causes of death and disability in developed economies such as the USA. With asthma being a chronic disease, it demands very much attention for a patient to undergo treatment. Since this disease is sensitive to environmental changes, records show that it has caused many death cases in certain seasons of the year. A study of such data is important while establishing the extent of the disease in a certain population. There are literature materials that have been established in a bid to study the effects of and what can be done to combat it. These form the basis of this paper as they are reviewed and analyzed. With asthma being a chronic disease, therapy is part of the medication process. To be precise, cell-based therapies are very important. Medical journals that address cell bases therapy as a remedy in asthma treatment have been used in this paper and the information they hold brought cohesion. As a result, a complete set of perfectly flowing information has been established.
Medical research has greatly advanced in the recent past. Many techniques have been developed to combat diseases that are resistant to conventional medication methods. Despite being a chronic disease, asthma has been incurable in most cases, but the story is changing due to the incorporation of cytotherapy. Cytotherapy or cell therapy has been undergoing thorough research and the advanced knowledge in this field has boosted the asthma remedy options.
To create an in-depth study of cell-based therapies as a remedy for asthma, it is a requirement that you first understand how asthma exists in a patient’s body. Asthma can be defined as the inflammation of the lungs. This is a disease that causes sensitivity to many environmental conditions like dust, pollen, and humidity. Afzal, Ramzan & Waqar (2020) explain that cell immunology has advanced greatly in the recent past. Diseases that had no cure are now curable. Chronic diseases can now be cured with a single medical operation. The beast behind these achievements is cell immunology. When the relationship between the cell and the immune system is established, it becomes very easy to pinpoint the affected cells and create a remedy based on several factors. The part of the body that is infected, the type of cells, the extent of infection, and the patient’s medical history are some of the factors that are examined to come up with a strategy to achieve the patient’s proper state of health. Since there is now extensive knowledge of how to carry out these medical operations, cell-based therapies gain more popularity. Cell-based therapies are even becoming the main focus for some medical institutions. Different chronic diseases can now be cured at a cheaper cost and using less time. These diseases have been consistently been a serious challenges in different parts of the globe. State governments have offered huge amounts of resources to focus on ways to treat these diseases. Research on these diseases has therefore had adequate resources for it to be effective. As a result, there have been many findings from this research. These findings are the main point of focus for this paper and they are reviewed from a biological perspective. Generally, the findings show positive progress and there is still a huge room for improvement.
Empirical Studies on Mesenchymal Stromal Cell Therapy
As previously noted, a great scholarly focus has recently been directed towards finding effective ways that can be used to treat asthma with many experts proposing positive cell therapies. A mesenchymal stromal cell has remained a great area of research for many years. Mesenchymal stromal cells have been identified and recommended by many healthcare researchers as a good intervention to treat asthma. This is informed by the reparative and immunological properties that they have as highlighted by Yao et al. (2018). According to a study conducted by Yao et al. (2018), it was determined that these cells are available in both the adult and neonatal tissues which makes them easy to target when treating asthma among patients of different ages. In a human body, they can be obtained from a range of areas including the bone marrow and adipose tissues. They are also available in other places like the lung and the umbilical cord. Nonetheless, it is necessary to point out that the MSCs can cause various anti-inflammatory or regenerative impacts that continue to present a challenge to many researchers (Yao et al. 2018).
Some recent studies have started conducting experiments to improve the action or effectiveness of MSCs as a potential treatment of asthma. For instance, the advanced BM-MSCs have been placed to test to determine how active they are in addressing asthma across populations of patients. In their study, Tynecka, Moniuszko, and Eljaszewicz (2021) indicated that directing these cells therapies to the vein help minimize eosinophilia. The same experiment further shown other important insights that are of great interest in the current cell therapy advancements. For instance, it was determined that the inhibition of Th2 and Th17 cytokines was initiated when this method was used showing a remarkable improvement in efforts towards addressing allegoric asthma. Another study that built on this also had phenomenal findings concerning the ability of these therapy options to deliver IT cells to the affected airways making it easier to arrest the condition and restore high-quality life to the patients (Tynecka, Moniuszko, and Eljaszewicz, 2021).
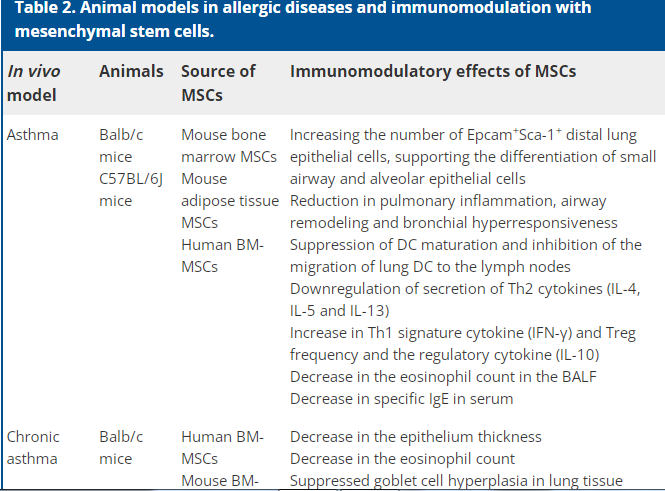
Fig 1: MSC’s Animal Model Immunomodulation
As shown above, several current studies have focused on testing animal subjects to understand how MSC acts on asthma patients and how immunomodulation happens. According to Ou-Yang, et al. (2011), the studies conducted on both animals and human subjects have indicated that sublingual immunotherapy, as well as subcutaneous immunotherapy, has high efficacies. They are also safe to use in the treatment of this condition. The secret behind immunotherapy has always been to initiate or evoke Treg cell generation. It also focuses on increasing tolerance of T lymphocytes that target a given allergen. In sublingual immunotherapy, the secretion of IL-10 is achieved by induction of T CELLS. When this induction is initiated, allergen-specific Treg cells generated enhanced levels of anti-inflammatory cytokines. Some of these include IL-10 and TGF-? (Ou-Yang, et al. 2011).
Further investigations have shown that there is a great challenge in studying MSCs and their performance in asthma and other allergic conditions. Some of the issues that pose great challenges to many researchers include ethical concerns and limited resources. It is also noted that the unknown side effects that might be experienced by the human subjects further discourage all-through research into MSCs. Available data suggest that intra-articular administration of MSCs in many animals is safe and can deliver the best outcomes. It is noted in some studies that problems such as tumor generation after the administration of MSCs were not observed. Nonetheless, caution must be exercised to ensure that there is no or limited contact with a serum to prevent virus transmission (Mitsialis & Kourembanas, 2016).
More researchers have come up and acknowledged the immunomodulatory benefits that come with the injection of MSCs during the treatment of allergic diseases including asthma. Specifically, the reduction of Th2 cytokine (IL-4), allergen-specific T-cell production, and increase of memory and naive T cells and Treg cells are some of the major properties that make these cells highly important in this endeavor. The regulation of allergen-specific T cells occurs through various responses. First, it involves the separation from Th2 to Th1 cell type (immune reaction). Second, it involves the initiation and facilitation of regulatory T cells (immune-regulation). In some findings, it is noted that
The in vitro immunomodulatory effect of DF-MSCs is another area that has attracted the attention of many researchers recently. Mitsialis and Kourembanas, S. (2016) noted that they profoundly suppress proliferative responses of CD4+ T cells, IL-4 and GATA-3 expression and this is property is what makes them quite important in this therapy. Most importantly, it was noted that this led to important outcomes such as reduction of effector and effector memory of memory CD4+ T cells. Moreover, it reduced antigen show-up stimulatory molecules on monocytes (Huleihel, Levine & Rojas, 2013). Some other studies have observed and indicated that an up-regulation of Treg cells and IL-10 levels is witnessed when the same process is followed.
As already been mentioned, MSCs are important in immune responses because of their ability and capacity to suppress activated T or B cells. They also can inhibit M1 macrophage differentiation, especially when responding to an antigen. According to Huleihel, Levine, and Rojas (2013), they are ideal candidates for therapy treatment due to their immunomodulatory action and multipotency. Recent studies have shown that the immunomodulatory action of these cells goes beyond allegoric conditions. They are beneficial in other areas such as neurodegenerative diseases, cardiovascular diseases, and autoimmune diseases. They can control immune reactions. It moderates T-cell production and controls the stability of Th1/Th2. At the same time, they improve the Treg regularity while controlling antibody production of B lymphocytes (Lange-Consiglio et al. 2019). Below is a presentation of MSCs action:
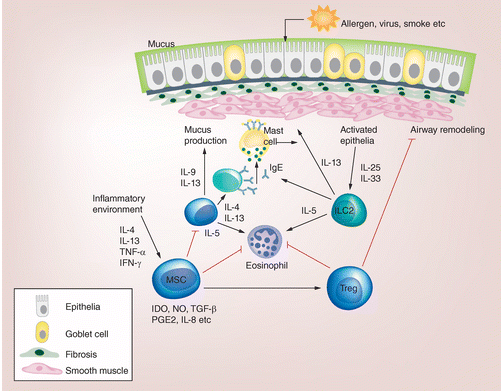
Fig 2: MSC’s the immunomodulatory action
Studies on OVA-Induced Asthma Model
Some of the studies have further indicated that ovalbium (OVA)-induced asthma is treated much better using this method. An investigation by Behnke et al. (2020) determined that the ability of the IT route to direct cells to the airways makes it possible to achieve a minimized level of eosinophilia. Among the patients treated with this therapy, it was determined that a substantial airway remodeling was noted just 14 days after the administration.
While the OVA-induced model is used by many clinicians across the realm of healthcare, its effectiveness has remained questionable prompting even deeper research studies. Some findings have shown that it is more appropriate to allergen and grass pollen. Some of the best options that have been suggested concerning this include house dust mite (HDM) which many researchers find relevant to humans. The biggest problem that many physicians and other personnel treating asthma is that administration of BM-MSCs may not be effective in some scenarios. For instance, its injection may not effectively prevent lung parenchyma inflammation. This makes it the least option or intervention when it comes to such problems even though it is quite important in some other situations. Such limitations have been considered by researchers in the past and determined that having a prior treatment intervention could help address this challenge. For instance, an experiment by some researchers recently indicated that having a prior treatment involving eicosapentaenoic acid (EPA) helps increase the effectiveness of this therapy. In their explanation, Du et al. (2018) offer a detailed explanation of why this combination would help potentiate the therapy. First, it allows for the inflection of macrophages directed to the anti-inflammatory phenotype (Du et al. 2018). It also leads to enhanced production of anti-inflammatory facilitators within the system.
In a more detailed observation of this therapy’s effectiveness, Gonzalez-Pujana et al (2020) brings up the issue of cockroach extract (CE) and how it facilitates asthma among young individuals. As an allergen, the best way recommended by many researchers is a model that is based on the CE-induced asthma approach. It is worth pointing out that the activation of the aryl hydrocarbon receptor (AhR) has also been identified as a great idea when it comes to improving BM-MSC functionality in asthma treatment. It has the potential of neutralizing environmental toxicity thereby making it much easier for the BM-MSC to function properly during asthma therapy. However, while the improvement that AhR offers to BM has been established, not much is known about its connection to MSC at a time of immunomodulation activity, something that further studies should seek to determine.
It has further been discovered that ADMSCs also play an important role in asthma therapies, especially with the new cell-based approaches used today. Their role is more pronounced because of their expansive immunomodulatory capacity. Various tests have been done to experiment on the therapeutic potential of ADMSCs using mice. It was noted that the subject had its CD4+CD25 + Foxp3+ Tregs ratio restored when injected with the chemical. This new balance informed the researchers that the therapeutic potentials of this chemical is high and can work well with humans. It has been shown in numerous studies that MSCs that are obtained from adult tissues may not be as effective given that their cell variability quality has deteriorated. It makes them inappropriate for use in cell therapies. This explains why many researchers suggest that MSCs that are derived from the placenta should work in case the stem, cells are unavailable. They tend to have all the needed ingredients that can help ensure that the therapeutic process runs smoothly. The recommended type is known as human placenta MSCs (hPMSCs).
The effectiveness of human placenta MSCs (hPMSCs) has been a matter of scientific concern for years. In one study, an hPMSCs from a healthy pregnant woman was extracted and administered to a rat. The subject was OVA-induced asthma. The aim was to show Th17/Treg balances or changes when this is injected. The findings indicate that there was a significant rebalancing which further led to an increase in IL-10 levels (Harrell et al. 2019). To understand this phenomenon further, other series of studies have tried to assess changes in the Notch pathway. This region is associated with the stimulation of Th2 in asthma. The findings indicated that there was a significant decrease when the injection was made after some days (Harrell et al. 2019).
A recent study focusing on the impact of human placenta MSC determined that the human amniotic membrane is one of the best regions to obtain mesenchymally. Understandably, it is the case because of the oxidation stress processes that happen in this part. However, it cannot be denied that there is the interplay of several other factors that lead to this nourishment and overall productivity of this region. Some of them include TGF-? and IgE whose increase or decrease causes a change of equal measure.
It is also noted by some other studies including Gurung et al (2018) that iPSC-MSCs have become even more important sources of mesenchymal capturing even greater attention today. They are considered more appropriate because of different reasons. First, they proliferate more than the MSCs. Second, they have higher differentiation ability and can live for far more periods than their counterparts Gurung et al. 2018).
Some other studies in this cell therapy have tried to examine the role of mitochondria and what mediates it to prevent what has come to be known as cell apoptosis within the epithelium layer. With the involvement of TNTs, it becomes easy to prevent airway inflammation that causes allergic reactions. It has also been discovered that collagen deposition and overall airway blockage is prevented if iPSC-MSC is injected into individual suffering from asthma. This explains why this model is highly effective in treating both acute and chronic asthma. These stem cells have remained advantageous because they do not present the threat of genetic instability. With such qualities, they have the capability of inhibiting Th2 and Treg cells. The mentioned cells are often the main target of asthma therapy.
However, it cannot be forgotten that the application of MSCs has shown great success in different animals. Regardless, there are myriad issues that have to be addressed if they are to be applied to humans. Most of these problems and challenges have been identified and documented in different research findings as discussed above. As of now, potentials or ability of MSCs in the treatment of asthma patients is still in question but that does not mean that clinical research breakthroughs that have been recently witnessed should be overlooked.
The greatest challenges that many of the clinical studies on the MSCS have included small sample sizes that make it difficult to generalize the findings with certainty to larger populations of asthma patients across the world. Moreover, the procedures for cell cultures are not yet standardized implying that any researcher can run a study that may not be replicated or redone by another to verify the findings. Generating an appropriate number of cells and having their regeneration properties retained requires a formal standardization that still lacks. Concisely, the biggest problem is having an efficient protocol that can guide further clinical research into this clinical problem. With this in place, it will be easier to harvest, culture, and present the MSCs that can ensure am effective therapy. More efforts need to be put to translate the animal model of MSC to the human version to protect many cancer patients, as suggested by Cereta et al. (2021).
Studies on Extracellular Vesicles
Extracellular vesicles (EVs) are important secretions that are also used currently in cell therapy of asthma. They are produced by various kinds of cells including the MSCs. Exosomes and microvesicles are some of the common examples of EVs. One of the major functions of these cells is communication and maintains a homeostatic balance within the extracellular system. Their properties are unique and highly sophisticated. The biological structures of these vesicles give them the great ability to initiate and sustain cell therapy in asthma. Some studies have further determined that several advantages are benefited when MSC-EVs are used instead of MSCs. First, the former is far much defined and less complex. Moreover, it is also easier to store them in facilities compared to MSCs.
The very initial study conducted on EVs indicated that its response to lung mechanism is entirely different from what is seen with MSCs. The study by Gonzalez-Pujana, et al (2020) further showed that the pro-inflammatory mediators’ reaction and the influence it has on T-Cells are also uniquely different. Even more interesting is the potentiality or the effectiveness of EVs that are obtained from hMSCs. They are far much potent and higher in effectiveness when used in asthma therapy models. However, their use has not been widespread as MSCs. Some experts encourage a campaign to investigate them further and use them more often in asthma treatments.
Type 2 airway allergic inflammation is a major concern that many researchers in this field have taken a keen consideration. It is caused by an enhancement of the level of ILC2s. To address this challenge and ensure that it can be arrested effectively, evidence has shown an intravenous treatment is necessary. It should involve the EVs that are obtained from iPSC-MSCs. To make this study credible and systematic, the scholars went ahead and defined a protocol for anion-exchange chromatography. The aim was to understand how the isolation process could be standardized in a way that allows anyone who would want to re-conduct the experiment to know how to go about it and receive the same results.
Many advantages come out when the ultracentrifugation protocol is used. First, the isolation process becomes defined and more clear making it easy to separate and obtain the necessary materials. This becomes even more beneficial in the industrial production of these resources. The isolation of MSC-EVs is a critical activity that requires well-stipulated and standardized approaches. The scalable and feasibility technique used in this approach would positively allow this to happen. This has been tested by many researchers including Gonzalez-Pujana, et al (2020). For instance, in the study, it was noted that the test groups indicated a reduction of M2 macrophages. It further suggested that EVs offer about 310 additional proteins that help in improving the effectiveness of cell therapy for asthma.
There are several other advantages associated with EVs as the best alternative to use in asthma treatment. A recent study connected the effectiveness of EVs to the abundance of miR-146a-5p in the umbilical cord. Moreover, the overall atmosphere where EVs are extracted makes it possible to find chemicals such as miR-146a-5p among others in abundance. Notably, these chemicals are important because they help remodel the air pathways such as while reducing inflammation. Importantly, oxygen depletion that is witnessed during asthma attacks is an essential player in the production of EVs. Therefore, it needs to be considered when utilizing this technique of treatment.
As previously mentioned, exosomes are some of the major types of EVs that are targeted when using extracellular vesicle (EV) therapy. Studies have shown that they present similar immunomodulatory impacts just like MSCs from where they may be obtained. However, the blood of patients with asthma at the PBMCs levels have do not necessarily have a connection with exosomes. Only vivo studies have established this relationship. In one study, the exosomes that are obtained from BM-MSCs are separated and cultured PBMCs (Gonzalez-Pujana et al. 2021). It is noted that this leads to a significant upsurge of various chemicals. Some of them include IL-10 and TGF-?1. This modulation is initiated by Tregs. However, the greatest challenge is that the exosomes present similar limitations just like those seen in BM-MSCs.
A similar study showed that hPMSCs administration is a great idea under various circumstances as long as some conditions are met. First, with children suffering from asthma, it is informed to reduce CD4+ and CD8+T activation. It is also important to consider decreasing IL-5 levels. Ultimately, the impact of asthma will reduce if IL-5 levels go down upon administration of hPMSCs under these circumstances. Considering the empirical evidence provided from these studies, it is clear that the EV-MSC therapy option is a great advancement that looks promising and may soon become the most reliable treatment of asthma. However, not enough data is available to make conclusive remarks and recommendations on how best this intervention can go. More studies are required to understand this therapy more in the future.
Immune Cell Treatment: T-Cells
Further studies have been conducted to understand how therapies that are focused on some other types of cells known as T-Cells can help in the treatment of this disease. The physio-biological response that occurs during an asthma attack has offered researchers important insights into how they can address this problem by focusing their attention on inflammatory, activated eosinophil and T cells. Primarily, T cells are important in ensuring that various antigens do not cause harm. They have been found to cause variation of CD4+ T cells breaking them into Th2 cells. These mentioned cells are unneeded because they prevent an immunological response of the T-cells making it hard to protect the body from diseases. However, inactivity of Tregs (being dysfunctional in a way that they cannot control Th-2) often leads to asthma. With this understanding, the therapy that includes or focuses on Tregs should aim at increasing their number and improving their ability to offer the suppressive role. This idea has been tested among several patients and has shown a promising outcome.
As noted by Gurung et al. (2018), one of the widely used techniques that involve Tregs is Antigen-specific immunotherapy (ASIT). The administration of this can take two forms, either SLIT or SCIT. However, the latter has shown far better outcomes when applied for Tregs-based therapy among asthma patients. Not much, however, is known about why this may be the case. What is in the open, according to Afzal et al. (2020), is that SLIT tablets are more applicable when house dust mite therapy is involved. Observably, the HDM SLIT tablet is responsible for various changes that are believed to help combat this condition. First, they influence the supply of fractional exhaled nitric oxide (FeNO). They are also effective in acting on airway inflammation. Ultimately, they help improve the airflow among patients leading to a direct enhancement of the quality of life of the sufferers.
A study on the impact of the administration of SLIT and SCIT among Chinese participants indicated a similarly high efficacy demonstrating that this is a great alternative therapy treatment that can be used worldwide among asthma patients. Notably, the researchers recommended that SCIT should be used as a supplement to pharmacotherapy. They did not recommend SLIT for the same indicating that the impacts of the two have varied significantly.
In ex vivo studies, Tregs were found CAR Tregs injected into animal subjects that had OVA-induced asthma had a high efficacy. This is since it was able to minimize Th2 and other forms of secretion leading to reduced airway activities and overall improvement. Like other forms of cell-based therapies, a more detailed and extensive study should be conducted on Tregs to advance its application in human patients.
Conclusion
Asthma has proven to be a killer disease that has been claiming many lives ever since it was first diagnosed. Attempts to prevent and treat it have been widely facilitated by the ever-advancing research studies. The emergence of different models and therapies that target the cells has shown significant outcomes. As shown in the discussion above, both human and non-human subject trial indicate that these treatments are highly effective strategies for asthma. However, the treatment options are not conclusive. As shown in the discussion, there exists a wide knowledge gap regarding cell therapy information. A lot of research and clinical trials are needed to understand some aspects of these treatments that focus on the cell, and how best to improve the quality of health of asthma patients. It is observed that most of the studies that have recently been conducted have used animal subjects and not humans. This further makes it difficult to positively translate the application of some of these models to human patients. Another observation is that the T-Cells are not well understood. The actual impacts of EVs have in different situations during cell therapy of asthma are yet to be determined through research. It has been shown that the interplay of these cells and their influence can be understood more deeply and responded to neutralize inflammation that is witnessed during asthma attacks. Lung function and health are critical that can be improved through careful and informed actions or interventions on these cells. While it is true that clinical research on these critical aspects or areas is still in the initial stages, a greater focus must be directed towards them as they hold key to the future of asthma treatment. The application of cell-based therapies described in this discussion is only an initial milestone to the development of asthma treatment. It is expected that a lot more advances will come as more in-depth research findings are continuing to emerge by the day. The ultimate aim is to enhance the well-being of asthma patients is on course and is expected to reach top-flight mode upon discovery of several other insights into how the mentioned challenges related to cell-based therapies of asthma.
References
Afzal, S., Ramzan, K., & Waqar, A. B. (2020). Alternative approaches for the treatment of Asthma and COPD: Focus on Cell-based therapies, Epigenetics, and Gene silencing approaches. Advancements in Life Sciences, 7(3), 181-189.
Behnke, J., Kremer, S., Shahzad, T., Chao, C. M., Böttcher-Friebertshäuser, E., Morty, R. E., … & Ehrhardt, H. (2020). MSC based therapies—new perspectives for the injured lung. Journal of clinical medicine, 9(3), 682.
Cereta, A. D., Oliveira, V. R., Costa, I. P., Afonso, J. P. R., Fonseca, A. L., de Souza, A. R. T., … & Da Palma, R. K. (2021). Emerging Cell-Based Therapies in Chronic Lung Diseases: What About Asthma?. Frontiers in Pharmacology, 12, 867.
Du, Y. M., Zhuansun, Y. X., Chen, R., Lin, L., Lin, Y., & Li, J. G. (2018). Mesenchymal stem cell exosomes promote immunosuppression of regulatory T cells in asthma. Experimental Cell Research, 363(1), 114-120.
Gonzalez-Pujana, A., Igartua, M., Santos-Vizcaino, E., & Hernandez, R. M. (2020). Mesenchymal stromal cell based therapies for the treatment of immune disorders: recent milestones and future challenges. Expert opinion on drug delivery, 17(2), 189-200.
Gurung, S., Williams, S., Deane, J. A., Werkmeister, J. A., & Gargett, C. E. (2018). The transcriptome of human endometrial mesenchymal stem cells under TGF?R inhibition reveals improved potential for cell-based therapies. Frontiers in cell and developmental biology, 6, 164.
Harrell, C. R., Sadikot, R., Pascual, J., Fellabaum, C., Jankovic, M. G., Jovicic, N., … & Volarevic, V. (2019). Mesenchymal stem cell-based therapy of inflammatory lung diseases: current understanding and future perspectives. Stem cells international, 2019.
Huleihel, L., Levine, M., & Rojas, M. (2013). The potential of cell-based therapy in lung diseases. Expert opinion on biological therapy, 13(10), 1429-1440.
Lange-Consiglio, A., Stucchi, L., Zucca, E., Lavoie, J. P., Cremonesi, F., & Ferrucci, F. (2019). Insights into animal models for cell-based therapies in translational studies of lung diseases: Is the horse with naturally occurring asthma the right choice?. Cytotherapy, 21(5), 525-534.
Mitsialis, S. A., & Kourembanas, S. (2016, April). Stem cell–based therapies for the newborn lung and brain: possibilities and challenges. In Seminars in perinatology (Vol. 40, No. 3, pp. 138-151). WB Saunders.
Ou-Yang, H. F., Huang, Y., Hu, X. B., & Wu, C. G. (2011). Suppression of allergic airway inflammation in a mouse model of asthma by exogenous mesenchymal stem cells. Experimental biology and medicine, 236(12), 1461-1467.
Tynecka, M., Moniuszko, M., & Eljaszewicz, A. (2021). Old Friends with Unexploited Perspectives: Current Advances in Mesenchymal Stem Cell-Based Therapies in Asthma. Stem Cell Reviews and Reports, 1-20.
Yao, Y., Fan, X. L., Jiang, D., Zhang, Y., Li, X., Xu, Z. B., … & Fu, Q. L. (2018). Connexin 43-mediated mitochondrial transfer of iPSC-MSCs alleviates asthma inflammation. Stem cell reports, 11(5), 1120-1135.
Yu, X., Yu, L., Guo, B., Chen, R., & Qiu, C. (2020). A narrative review of research advances in mesenchymal stem cell therapy for asthma. Annals of Translational Medicine, 8(21).

Time is precious
don’t waste it!

Plagiarism-free
guarantee

Privacy
guarantee

Secure
checkout

Money back
guarantee






