Infectious Arthritis Complete Margins, Thesis Paper Example
Abstract
Infectious arthritis is an infection in the joint fluid and joint tissues, specifically located in the synovial region. The infection usually reaches the joints though the bloodstream, although some joints may become infected due to an injection, surgery, or injury. Different bacteria and viruses can infect a joint and usually are associated with a person’s age, as well as other triggers. The purpose of this research is to identify the core causes of infectious arthritis, as well as contemporary treatments for prevention and symptom reduction.
Introduction
Infectious arthritis is a pain, aching, or swelling mostly developed in joints. This form of infection is usually caused by a viral, bacterial, or fungal infection that spreads to the meeting point of two joints like the knees or elbows. In addition to the traditional inflamed joint swelling and aching, infectious arthritis can cause symptoms like fever and chills. The most frequently effected joint is the knee.
What is infectious arthritis?
Septic, or infectious, arthritis is an infection of the joints. This is usually caused by by microorganisms, and results in the joint being coated with inflammatory or acidic fluid that eats away at the bone marrow due to microbes present in the joint fluid. This fluid, known as synovial fluid, or joint fluid When normal joint fluid is sterile,, if it were removed and cultured in the laboratory, no microbes would be found. In diagnosing most cases of infectious arthritis, , microbes are clearly recognizable in affected joint fluid. In most cases, infectious arthritis affects a single joint, but occasionally more joints are involved. Affected joints vary depending on how reactive the arthritis might be and the microbes causing the infection.
Reactive Arthritis
One type of infectious arthritis is reactive arthritis. Reactive arthritis is the inflammation of a joint in reaction to a bacterial, viral or fungal infection. Often reactive arthritis occurs due to an infection in the body located somewhere completely unrelated to the effected joint. While the effected inflamed joint is usually located in the knee or toes, the actual infection causing the symptoms can stem from e. Infections that causes reactive arthritis are usually developed in the vagina for women, or the bladder, urethra, or urine tube for men. Reactive arthritis also commonly spawns from food-born bacteria, or sexually transmitted infections.
History/ Discovery
Historical record of arthritis cases have been compiled by archeologists and medical professionals to trace the origin of the ailment. Primary ankle osteoarthritis was discovered in dinosaurs. The first documented cases of human arthritis dates back to 4500 BC. It was discovered in the skeletal remains of Native Americans. These particular remains were found in Tennessee, more cases of arthritis were found in Olathe, Kansas. 500 BC marks the moment when willow bark was identified as a cure for aches and pains caused by arthritis. 2000 years later, around 1820 salicin was discovered to be the chemical in willow bark that treats arthritis. The problem was that the compound turned out to cause nausea in patients. Following up on this discovery, 80 year later, Felix Hoffman of the Bayer Company discovered a method of isolating salicin to utilize its effects without having to deal with the nauseating effects. Before this discovery, Bayer Company specialized in dye production and this finding opened up a promising market for the company that resulted in the Bayer pain relief products for which the company is currently known. The story is that Hoffman, in an attempt to create a cure for his father’s chronic arthristis, discovered a way to isolate the compound which The Bayer Company trademarked in 1899 and called Aspirin.
Etiology
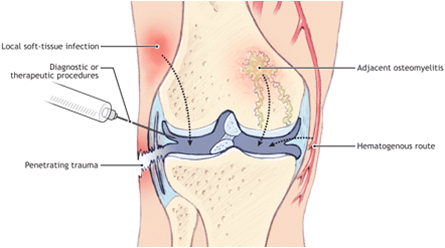
In regards to European cases of arthritis, the most common etiological causes of virtually every infectious arthritis incident is nongonococcal. All cases in the United States are caused by Staphylococcus aureus (Shirtliff & Mader, 2002).Authors note that,“The representation of S. aureus is more pronounced in patients with either rheumatoid arthritis or diabetes (Shirtliff & Mader, 2002).” The authors note that the synovial membrane is vulnerable to the entry of bacteria because it has no basement plate as stated in their study, “The synovial membrane has no limiting basement plate under the well-vascularized synovium; this allows easy hematogenous entry of bacteria (Shirtliff & Mader, 2002).” This easy access to numerous vulnerable body entry points explains why infectious arthritis is so common.
Who is at risk of developing infectious arthritis?
Joint infection rarely affects people who don’t have any documented predisposing risk factors. It usually develops in an environment where there are risks that pose the potential of developing infectious arthritis. These are specific risk situations, like ”taking medications that suppress the immune system, intravenous drug abuse, past joint disease, injury, or surgery, and underlying medical illnesses including diabetes, alcoholism, sickle cell disease, rheumatic diseases, and immune deficiency disorders (Shirtliff & Mader, 2002).” People with these specific conditions have a higher probability of developing infectious, or septic, arthritis
Symptoms
Septic arthritis is usually caused by viruses bacteria, and fungi. Bacteria is the leading and most common cause of septic arthritis. This includes Staphylococcus aureus and Haemophilus influenza. High-risk patients, are vulnerable to other forms of bacteria that can cause infectious arthritis such as E. coli and Pseudomonas, which is common among drug abusers who use intravenous methods. The elderly tend to contract Neisseria gonorrhoeae in the sexually, and and Salmonella. . In young children, individuals with sickle cell can be vulnerable to other bacteria that can cause infectious arthritis include Mycobacterium tuberculosis, or spirochete bacterium. Both these forms of bacteria can also incite Lyme disease, which. The most common Viruses that can cause septic arthritis include hepatitis A, B, and C , parvovirus B19, herpes viruses, HIV (AIDS virus), HTLV-1, adenovirus , coxsackie viruses , mumps, and ebola . The noted fungi that can develop into septic arthritis include histoplasma , coccidiomyces, and blastomyces. Infectious arthritis symptoms are fever, chills, as well as joint pain, swelling, redness, stiffness, and warmth. Large joints are the ones most commonly vulnerable to infectious arthritis. These joints include knees, hips, elbows and ankles. Candidates with high risk factors like infections of certain joints, or pre-existing inflammatory arthritis related infections like those caused in the collar bone, or sternum are vulnerable to uncommon microbes such as Brucella and they can contract infectious arthritis as well. Core symptoms of all these patients tend to be inflammatory reactions such as swelling in the affected area, but in high risk severe cases the infection can result sin deformity of the joints and even death.
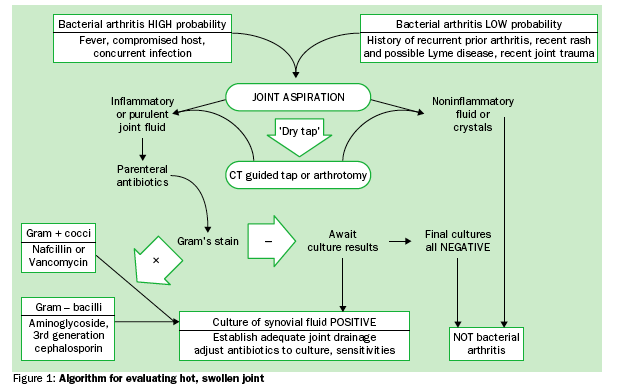
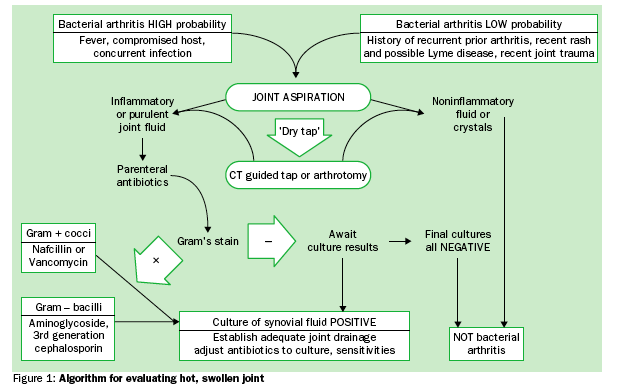
Diagnosis
To diagnose infectious arthritis, healthcare providers test blood, urine, and joint fluid. Treatment medicines and sometimes surgery. Infectious arthritis is usually diagnosed as infected joint fluid. Joint fluid is removable with a needle or syringe. Joint fluid is assessed in a lab; if it’s determined that there is an exceptionally high number of than it will be concluded that inflammation has occurred. A sample of joint fluid can show the lab professionals which specific microbe caused the infection and help them determine if it is susceptible to antibiotics. X-ray studies a particular joint can locate injuries in bones that are adjacent to the initial source of pain, but MRI is not traditionally used to diagnose cases of infectious arthritis. sedimentation rate, and C-reactive protein.
Rheumatoid arthritis (RA) is a chronic inflammatory disorder that can significantly damage tissue, bones and organs after attacking flexible synovial joints if not diagnosed early on and treated effectively.
Appropriate laboratory and/or radiological tests
Diagnosis of infectious arthritis in rheumatoid patients, tends to get prolonged, which results in a notably worse outcome in comparison with other patients with septic arthritis (Al-Ahaideb, 2008). A common diagnosis of rheumatoid patients susceptible to infectious arthritis is the pre-existing development of lesions or abnormal joint structure (Al-Ahaiden, 2008). In cases of rheumatoid arthritis identifying the cause, or onset of infectious arthritis is very complicated and difficult, most likely because as the Goldenberg notes, “Septic arthritis is most likely in patients with longstanding rheumatoid arthritis (panel 2), and in such patients treatment is often delayed because it is wrongly assumed that the joint symptoms are related to an exacerbation of the underlying rheumatoid arthritis (Goldenberg, 1998).” The author goes on to note that the complexity of identifying cases like these stems from what is considered to be the standard diagnosis process for infectious arthritis onset.
The typical patient diagnosed with infectious arthritis starts with an acute onset of severe joint pain, which is then exacerbated by limited mobility, and accompanied by swelling and erythema of the effected joint (Al-Ahaideb, 2008).The particular cause of infectious arthritis, whether it’s viral, fungal, or bacterial is not always easily diagnosed, as one author notes, “The definitive diagnosis of bacterial arthritis requires identification of bacteria in the synovial fluid by Gram’s stain or by culture.Most infected joint effusions are purulent or very inflammatory with an average leucocyte count of 50–1503109/L, predominantly polymorphonuclear cells (Goldenberg, 1998).In cases of acute infectious arthritis, radiographs can’t identify destructive joint lesions but are useful in determining a joint effusion and in demonstrating concurrent osteomyelitis or arthritis (Goldenberg, 1998).
The most severe case of infectious arthritis are those seen developed in rheumatoid patients. “The patient will often be afebrile and the presentation indolent. Diagnostic delay is an important contributor to the poor outcome of septic arthritis in rheumatoid arthritis, which carries a 30–50% case-fatality rate (Goldenberg, 1998).”Incidents of bacterial arthritis have led to what is considered the most severe form of arthritis, rheumatoid, have been reported in large numbers in “Scandinavia and Australia at 5.7 to 9 per 100, 000 person-years and in England at 1 in 49, 000 per 100 000 person-years, with increased incidence in patients with rheumatoid arthritis and joint prostheses (Margaretten, Kohlwes & Moore, 2007).” As this form of arthritis can be fatal, the indication represents the need for urgent and quality care on a global scale. Patients with rheumatoid arthritis, which is also known as joint prostheses, because the joints become unusable, tend to have a higher chance of experiencing infectious arthritis, but as the authors note, “distinguishing infection from underlying arthritides creates diagnostic challenges and a heightened urgency (Margaretten, Kohlwes & Moore, 2007).” This heightened urgency is most common in only the most severe cases, specifically rheumatoid arthritis induced infectious arthritis.
In more common cases like gonococcal arthritis, where women are affected 2 to 3 times more frequently than men, the actual possibility for limb deformity is rare. Despite this , medical professionals note that in these cases, “migratory tenosynovitis often accompanies the arthritis (Margaretten, Kohlwes & Moore, 2007).” This is also a common cause of the formation of septic joint development. Hospitals have reported that most septic joints are infected due to hematogenous seeding of the vascular synovial membrane, which is usually caused from a bacteremic episode. They also believe that this can form from a local . corticosteroid joint injection (Shirtliff & Mader, 2002).
Treatments
Treatment of acute bacterial arthritis demands the use of antibiotics and constant joint drainage . Authors note, “the initial choice of antibiotics should be based on the Gram’s stain and the age and risk factors of the patient (Goldenberg, 1998).Shorter paths to treatment in the form of oral antibiotics have been proven to be very effective in treating children or adult women with gonococcal arthritis, which are the two most common cases to date. The authors note that in these cases, tntraarticular antibiotic instillation is not required and such therapy may cause a chemical synovitis (Goldenberg, 1998).” Here the authors note that overtreatment of mild infectious arthritis cases can results in chemical poisoning of the patient. For this reason often surgical drainage is carried out to prevent the possibility of chemical synovitis. For these particular treatment cases, it’s noted that, “Patients should be initially treated with needle aspiration if a joint infection is easily accessible, if the vast majority of the purulent fluid can be removed, and if the patient does not suffer from negative prognostic indicators (Shirtliff & Mader, 2002).” It is up to the particular doctor handling the case to identify the particular bacterium that’s causing the infection. Once this bacterium is identified, most effective antibiotic can be selected to target the specific cause of the problem. Antibiotics are usually given through a vein in the arm. This is known as intravenous administration. The Mayo Clinic staff note that, “The most common method of removing joint fluid is through arthroscopy (ahr-THROS-skuh-pee). In arthroscopy, a flexible tube with a video camera at its tip is placed in your joint through a small incision (Mayo Clinic staff, 2010).” The most fatal and severe cases of infectious arthritis are those caused by rheumotaoid arthritis and they are also the most critical to treat. In these cases it is not considered safe or preferred to drain the fluid intravenously. The Mayo Clinic staff note that, “It is thought that surgical drainage may provide the patient with increased joint protection and is often the preferred mode of treatment in the patient with rheumatoid arthritis due to their increased susceptibility to joint damage (Al-Ahaideb, 2008).” It is the common belief among many medical professionals that in treating infectious arthritis, no standard method has been established in the aspect of which particular antibiotic is best for treatment. In these case the selection of the antibiotic is up to the discretion of the medical professional overseeing the procedure, and they tend to base this decision on “suspected organism and local sensitivity and resistant pattern (Muhayidin & Said, 2009).”
Prognosis
One of the most noted complications of infectious arthritis is the need for rapid clearing of the infection, as it is critical to prevent joint damage. Antibiotics are usually administered immediately so that joint integrity can be sustained throughout treatment. Losing limb functionality is a high possibility, so these treatments are not taken lightly. In all cases of infectious arthritis, the chance for limb destruction exists, especially if the infection has been long-standing. Mayo Clinic medical practitioners note that when treating infectious arthritis, “the keys to successful outcome are rapid medical attention and drainage and the accurate administration of antibiotics to which the offending microbes are susceptible (Mayo Clinic staff, 2010). If infectious arthritis is diagnosed at an early stage and treated periodically, one can prevent joint damage. In every case of infectious arthritis, joint damage is always a possibility. This is specifically true with bacterial infections.
Since bacterial infections, are the core cause of infectious arthritis, they tend to be treated first and foremost with antibiotics. First the synovial fluid harboring the infection is drained from the joint and the antibiotics are either injected or ingested. In a hospital setting, due to the fact that the treatment of antibiotics must be done efficiently and periodically over time, the dosages are often administered intravenously. The specific choice of antibiotic is dependent on the culture of the joint fluid and this is measured through testing. As studies show, “until those results are known, empiric antibiotics are chosen to cover a wider range of possible infectious agents. Sometimes, combinations of antibiotics are given. Antibiotics can be required for four to six weeks (Mayo Clinic staff, 2010).” The most important aspect of all this is the act of drainage. When the patient has their joint drained on a continuous basis, it means rapid clearing of the infection from the affected area. This prevents the possibility for any developing or reoccurring damage to the joint tissue. Permanent damage could manifest itself in the form of limb deformity. On the drainage process healthcare professionals note that, “drainage can be done by regular aspirations with a needle and syringe, often daily early on, or via surgical procedures. Arthroscopy can be used to irrigate the joint and remove infected joint lining tissue.”This is the standard method for drainage, but in some extreme cases this method is not adequate enough to prevent the recurrence of infected fluids, or even the initial complete drainage of infected fluids. In these case the authors note that, “If adequate drainage cannot be accomplished with joint aspirations or arthroscopy, open joint surgery is used to drain the joint. After arthroscopy or open joint surgery, drains are sometimes left in place to drain excess fluid that can accumulate after the procedure (Mayo Clinic staff, 2010).”
Data & Other Findings
Documented data in regards to infectious arthritis has developed and expanded throughout the years. This is the information that best paints a clear understanding of current developments and progressions. U.S. based health statistics in regards to infectious arthritis stemming from those patients with pre-existing inflammatory arthritis found that as documented by researchers Kherani and Shojania “The annual incidence of septic arthritis in the general population is 2 to 5 per 100 000. Patients with inflammatory arthritis are predisposed to septic arthritis (Kherani & Shojania, 2007).” “Although the knee is most commonly affected, other large and medium joints can also be affected (Kherani & Shojania, 2007).”As noted by retrieved data, “the diagnosis of mycobacterial or fungal arthritis should be entertained when a patient presents with chronic monarticular arthritis. Both of these arthritides have increased in prevalence, largely due to increased incidence rates seen in HIV-infected patients (Shirtliff & Mader, 2002).”There is a higher incidence of infection in people who ingest steroids, but data notes that, “50% of patients with rheumatoid arthritis who developed polyarticular septic arthritis (PASA) were not receiving steroids (Al-Ahaideb, 2008).Septic arthritis is also notably more common in children candidates than grown adults. The reason for this is actually unknown (Scarfone, 2011) There are a higher number infectious arthritis cases reported in young boys rather than girls (Scarfone, 2011).As previously noted, infectious arthritis is most common among younger individuals, specifically younger than 3 years of age (Scarfone, 2011). The following represent the percentages of young children who have reported cases of infectious arthritis in relation to other conditions.
Across the board, the most standard and common cause of infectious arthritis in the largest pool of those stricken with infectious, young children age 1-3, meningococcal bacteria was found as the core triggering cause. As the authors noted in a study of all case pertaining to this infected group, “Meningitis (10-30%), osteomyelitis (5-10%), cellulitis (10-30%), and pneumonia (5%) are potential complications in young children with septic arthritis resulting from hematogenous spread of H influenzae type B (Scarfone, 2011).” In cases regarding young adults that were sexually active the authors note that,“The commonest cause of septic arthritis in sexually active young adults is N. Gonorrhoeae(i.e 75% of cases) (Muhayidin & Said, 2009).” They further go on to indicate that older adults are the ones who endure roe sever cases as, “In older adults, Staphylococcus aureus account for almost 80% of patients with polyarticular septic arthritis and 62% with monoarticular septic arthritis (Muhayidin & Said, 2009).” This is a tragic statistic as staphylococcus is a more deforming and possibly fatal form of infectious arthritis. This is why as some authors note fatally from infectious arthritis is a major concern.
In their study on infectious arthritis patient mortality rates, researchers and medical professionals Muhayidine and Said note that “Despite antibiotic era and better access to medical facilities, the mortality and morbidity from septic arthritis is still high. Dubost found up to 30% mortality rate in patients with polyarticular septic arthritis either due to the infection or as a consequence of the disease. (Muhayidin & Said, 2009).”
Conclusion
In sum, infectious arthritis is a symptom of numerous physical ailments, and while it is curable and preventable it is not to be taken lightly. Whether a patient is suffering from a more standard functional class of infectious arthritis like bacterial meningococcal, or the more severe and deforming rheumatoid, the treatment necessities are the same, early diagnosis and rapid treatment. Many rheumatoid patients have demonstrated, delayed diagnosis can be fatal. This was clearly noted by Al Ahaideb when he said, “It is very crucial to reach the diagnosis of septic arthritis in an early stage in any case but in particular, in immuno-compromised patients like the rheumatoid patients. Late diagnosis may lead to disastrous sequale (Al-Ahaideb, 2008).”All research presented proves that bacterial arthritis outcomes have not changed much in the past few decades. This is despite the implementation of numerous new effective antibiotics and advanced tools for joint drainage (Goldenberg, 1998).Outcome directly relates to multiple factors, such as prior damage to joints, and or potential surrounding risks that have created an environment of virulence of the infected organism (Goldenberg, 1998)All studies suggest that the key to proper treatment and prevention rest in the practice of early diagnosis and rapid medical attention, and timely drainage of joints in supplement to continuous use of antibiotics.
The cases of infectious arthritis that have resulted in deforming patients tend to be the most inflammatory while the more standard cases are of, or similar to, the bacterial meningococcal class. Many of the studies found that functional outcomes of arthritis in bacterial meningitis are generally good because meningococcal arthritis is usually immune-mediated, and pneumococcal arthritis is generally less deforming than staphylococcal arthritis (Weisfelt, Van de Beek, Spanjaard & de Gans, 2006).” This simply points to the fact that the bacterial meningococcal class of infectious arthritis is a functioning form. This class, as the studies have shown happens to be the standard bacterial form just spread in different class structures. Collective studies found that infectious arthritis is a common development an many naturally occurring bacterial illnesses like community-acquired bacterial meningitis. While it was found to be was diagnosed in 7% of patients (Weisfelt, Van de Beek, Spanjaard & de Gans, 2006), this key statistic along with the wide range of other bacterial, fungal, and viral factors that influence infectious arthritis paints a clear picture that there is no discrimination among candidates or severity for this ailment Treatment of infectious arthritis is a global concern one that can be the difference between ensuring a patient has a more comfortable quality of life, or in some case that the patient can have a life at all. While most studies have show documented cases have been light, it’s still not to be taken lightly in regards to diagnosis and rapid treatment.
References
Goldenberg, D. L. (1998). Septic arthritis. The Lancet, 351, 197-202.
Margaretten, M. E., Kohlwes, J., & Moore, D. (2007). Does this adult patient have septic arthritis?. JAMA,297(13), 1478-1488.
Bramble, A. (Photographer). (2012). Septic arthritis. [Print Photo]. Retrieved from http://www.physio-pedia.com/File:Septic_Arthritis.png
Shirtliff, M. E., & Mader, J. T. (2002). Acute Septic Arthritis. Clinical Microbiology Reviews, 15(4), 527-544.
Mayo Clinic staff. (2010). Septic arthritis. Mayo Clinic, Retrieved from http://www.cnn.com/HEALTH/
Shiel , W. C. (2008, May 12). Septic arthritis. Retrieved from http://www.medicinenet.com/septic_arthritis/article.htm
Al-Ahaideb, A. (2008). Septic arthritis in patients with rheumatoid arthritis. Journal of Orthopaedic Surgery and Research, 3(33)
Scarfone, R. J. (2011, July 29). Pediatric septic arthritis. Retrieved from http://emedicine.medscape.com/article/970365-overview
Weisfelt, M., Van de Beek, D., Spanjaard, L., & de Gans, J. (2006). Arthritis in adults with community-acquired bacterial meningitis: a prospective cohort study. BMC Infectious Diseases, 6(64)
Muhayidin, A. D., & Said, M. S. M. (2009). Septic arthritis in rheumatology:review of five cases .Journal of Clinical Medicine Research, 1(3), Retrieved from http://www.jocmr.org/index.php/jocmr/article/viewarticle/86/92
Kherani, R. B., & Shojania, K. (2007). Septic arthritis in patients with pre-existing inflammatory arthritis.CMAJ, 176(11), 1605-1608.
(Goldenberg, 1998)
(Goldenberg, 1998)
(Bramble, 2012)

Time is precious
don’t waste it!

Plagiarism-free
guarantee

Privacy
guarantee

Secure
checkout

Money back
guarantee






