Autogenous Tooth Transplantation: Five -Year Re-Evaluation of a Vital Transplant, Case Study Example
Abstract
Autogenous tooth transplantation or the surgical movement of a tooth form one location to another in the mouth in the same individual is considered as an excellent option when the conditions are right for tooth replacement. This procedure was at one time considered as experimental however, autogenous tooth transplantation can provide a functions and esthetic result for tooth replacement under the proper indications. Clinical evidence required in successful tooth transplants is inclusive of a periodontal ligament, no root resorption and no evidence of ankylosis. The transplantation reported in this study involved the extraction of a single-rooted maxillary anterior supernumeracy lateral incisor donor tooth following the preparation of the recipient socket site at the location of the congenitally missing mandibular central incisors.
Introduction
The concept of tooth transplantation for many is not realistic due to the narrow indications for its use. Required is strict selection of patients combined with appropriate surgical technique for success to be realized. The consideration of the transplant as a clinical option has been eliminated due to the predictability of implant dentistry. However, the long-term prognosis of dental implants in addition to how these implants accommodate to the changing natural dentition during the process of aging is yet unknown. This study re-evaluates the autogenous tooth transplant and the role it may play as a treatment plan option. In addition, this study highlights the indication for autogeneous tooth transplantation using a case report as an example. Review of the recommended surgical technique and success rates will be discussed.
According Andresen, et al ( 2001) (1) results reported in a long term study of 370 transplanted premolars, the state of most development that is optimal for this procedures is “three-quarters root formation in which the apex is wide open and the follicle covering the root surface is thick and resistant to trauma.” (Andresen, et al, 2001, p.134) When the transplantation has been carried out It is very important to monitor eruption and periodontal and pulpal healing.” (Andresen et al, 2001, p.134) Eruption will take place after several months, periodontal ligament healing can be verified after six weeks. (Andresen, et al, 2001, p.134) The growth of additional root can be verified in the majority of cases however, in approximately one-third of transplanted premolars there will be arrest of root formation results. If the tooth is graphed after 75% root formation has taken place there will generally be no practical implications for the long-term survival of the implant. (Andresen, et al, 2001, paraphrased) This procedure is highly predictable and dependent on the state of root formation, which has been confirmed during long-term studies. (Andresen, et al, 2001, paraphrased)
For many, the concept of tooth transplantation may not be realistic due to the narrow indications for its use. Strict patient selection in addition to appropriate surgical technique is required for success. The predictability of implant dentistry has virtually eliminated consideration of the transplant as a clinical option. However, the long-term prognosis of dental implants and how they accommodate to the changing natural dentition during the aging process yet remains to be seen. This paper re-evaluates the autogenous tooth transplant and the role it may play as a treatment plan option. This article highlights the indication for autogenous tooth transplantation using a case report as an example. Review of the recommended surgical technique and success rates will be discussed.
Work by Apfel, Hale and Miller in the 1950’s was the first to well document the successful autogenous tooth transplant and establish the surgical techniques along with indications for autogenous tooth transplantation. Third molars with incomplete root formation were moved to other sockets of extracted teeth and as by the high success rate reported in the studies over the last decade autogenous tooth transplantation has demonstrated to be a viable option for tooth replacement under the right condition.
Background
The work of Clokie, Yau, and Chano (2001) (3) entitled “Autogenous Tooth Transplantation: An Alternative to Dental Implant Placement” reports that the earliest reports of tooth transplantation occurred in slaves in ancient Egypt who were compelled to provide their teeth to the pharaohs. This procedure is reported as having been abandoned due to “problems of histocompatibility” and this was replaced with autotransplantation. (p.92) Patient selection is of critical importance in successful autotransplantation. Patients must be healthy and capable of following post-operative instructions and able to keep follow-up appointments. In addition, patients should “demonstrate an acceptable level of oral hygiene and be amenable to regular dental care.” (Clokie, Yau, and Chano, 2001. (p.93)(3) The most important factor is the patient having a suitable recipient site and donor tooth. (Clokie, Yau, and Chano, 2001, p.93) (3)
Dentistry has been historically primary concerned about tooth extracting and provision of prosthesis for edentulous areas. In the past, animal teeth, ivory, bone and human teeth extracted from the deceased has been sued as denture material but due to discoloration none of these material were found acceptable with reasons stated as “discoloration, bad odor and structural weakness.” (Andreason, 2001, p.170) Tooth transplantation was conducted exclusively on the upper classes until the latter part of the 19th century, since only the upper classes could afford such treatment. In the 1950s information about autotransplantation began to appear with the concept being that following extraction of a first molar that was unrestorable due to severe decay that an impacted developing third molar could be transplanted to replace the extracted tooth with a 50% success rate. Failure was due to the lack of development of the transplanted tooth and autotransplantation was then considered only a temporary treatment. Autotransplantation has gained attention since recent research on periodontal ligament healing following autotransplantation has made provision of information that can be applied to the procedure.
Case Report
During a routine orthodontic examination of an 11-year male it was found that both lower mandibular central incisors were congenitally missing. The patient was referred for evaluation of an erupting maxillary single rooted supernumerary tooth in the buccal vestibule adjacent to tooth #10, class III mobility of the retained primary mandibular central incisors and congenitally missing mandibular central incisors 24 and 25. Radiographic examination revealed a retained primary dentition at the sites of congenitally missing teeth 24 and 25 in addition to the presence of a maxillary single rooted supernumerary tooth with incomplete root formation.
Since the maxillary supernumerary tooth was to be extracted, it was decided to attempt an autogenous tooth transplant of the upper supernumerary single rooted tooth to site of the retained primary and congenitally missing central mandibular incisors. The space allotment would require enamel plasty of the maxillary supernumerary tooth prior to inverting and planting into the recipient site.
Indications
Qualities of candidates for autogenous tooth transplantation include patients who are systemically in good health and acceptable for oral surgical procedures; show good oral hygiene practices; have donor teeth and who choose autogenous tooth transplant procedures over other treatment modalities. Indications for donor teeth include adequate viable periodontal ligament and that can be extracted with minimal damage to the periodontal ligament. Single rooted teeth without surface concavities are the best candidates. Nonworking, mal-positioned, dislocated, tilted or impacted teeth qualify well. Recipient site indications include alveolar ridges with sufficient height and width to receive the donor tooth or teeth.
Contraindications
Low position of the maxillary sinus and high mandibular canal are contraindications. Transplant procedures may cause infections to a recipient site if gingival closure is not achievable. Other contraindications include patients with poor home care and compliance; systemic health concerns that do not permit surgical procedures; who have no donor teeth or acceptable recipient sites; and who want other treatment options that might be available.
Surgical Technique
The autogenous transplant was completed according to the following sequence:
(1) local anesthesia was provided at the donor site and recipient site;
(2) radiographic measurement of the root form;
(3) enamel-plasty of the clinical crown of the donor tooth according to the space requirements of the recipient site;
(4) preparation of the recipient socket with a trephine and aqueous amounts of irrigation;
(5) extraction of the donor tooth;
(6) inversion and insertion of the donor tooth into the recipient site;
(7) soft tissue closure was completed using a resorpable suture achieving soft tissue contact around the neck of the transplanted tooth;
(8) rigid splinting to the adjacent dentition and occlusial evaluation and adjustment was completed using a high-speed finishing bur;
(9) antibiotics and post-surgical instructions were given to the patient and parents.
Attention was given to minimize the trauma to the periodontal ligament at the time of extraction and positioning at the recipient site. Donor tooth extra-alveolar time was limited to seconds and the splinting duration was eight weeks. Splinting was comprised of extra-coronal composite material involving the adjacent dentition.
A soft diet should be followed for several days following surgery.
During the healing period the tooth should be evaluated for the onset of pulpal necrosis as seen by periapical radiolucency, the presence of a draining fistula, radiographic root resorption, or intra-pulpal calcification.
Autogenous transplants with incomplete apexification may remain vital following the transplant procedure. Developing teeth with open apices may not require endodontic treatment due to the potential for re-vascularization and re-innervation.
Literature Review
Donor Teeth Placement and Condition
It is reported in the work of Clokie, Yau, and Chano (2001) (3) that the donor tooth “should be positioned such that extraction will be as atraumatic as possible. Abnormal root morphology, which makes tooth removal exceedingly difficult and may involve tooth sectioning, is contraindicated for this surgery.” (Cohen, Shen, and Pogrel, 1995 (4) cited in (3) Yau, and Chano, 2001, p.94) In addition, it is reported that donor teeth may either be those with open or closed apices. (Clokie, Yau, and Chano, 2001, p.94) (3) However, it is stated that the best results are obtained “with teeth having between one-half to two-thirds completed root envelopment.” (Clokie, Yau, and Chano, 2001(3) , p.94; Cohen, Shen and Pogrel, 1995(4) ; Lundberg and Isaksson, 1996 (8); Kugelberg, Tegsjo, and Malmgren, 1994 (6) Kahnberg, 1987 (5) ; Norway and Konigsberg, 1980 (11); and Schwartz, Bergman, and Klausen, 1985 (14))
Root Formation
It is reported that surgical manipulation of teeth having less than one-half root formation is likely to be “too traumatic and could compromise further root development, stunting maturation or altering morphology.” (Clokie, Yau, and Chano, 2001, p.95 (3) When root development is more than two-thirds, it is reported that the increased length “may cause encroachment on vital structures such as the maxillary sinus or the inferior alveolar nerve.” (Clokie, Yau, and Chano, 2001, p.95(3) When the tooth has complete or nearly complete formation of its root canal therapy will be generally required and the tooth with an open apex “will remain vital and should continue root development after transplantation.” (Clokie, Yau, and Chano, 2001, p.95(3)
The Procedure
The procedure involves administering local anesthesia either alone or combined with some other type of sedation. Following sedation, the tooth at the recipient site is extracted and the socket prepared. Labiolingual and mesiodistal dimensions are determined through use of occulusal and periapical radiographs. (Clokie, Yau, and Chano, 2001, paraphrased) This information is used by many practitioners to ‘fabricate an acrylic replica of the tooth to be replaced. This replica allows them to prepare the recipient site using a guide with dimensions similar to those required for the donor tooth.” (Clokie, Yau, and Chano, 2001, p.95(3)
The next step is preparation of the donor tooth through careful removal to make sure there is the least possible trauma to the periodontal ligament. The donor tooth is then unerupeted and extraction includes elevation of flap, followed by removal of bone and next gentle follicle removal from around the crown. (Clokie, Yau, and Chano, 2001, p.95(3)
It is noted that a traumatic injury to the surface of donor tooth root will “impair the success of the transplant due to inadequate periodontal ligament regeneration.” (Clokie, Yau, and Chano, 2001, p.95(3) The donor tooth is handled as little as possible and only the cover should be carefully touched. Next, the tooth is placed in the recipient socket with “minimal delay between extraction and transplantation” which will ensure that the periodontal membrane vitality is maintained. (Clokie, Yau, and Chano, 2001, paraphrased)
Transplantation in Children with Accidental Teeth Loss
Transplantation of premolars should be a consideration in cases of children with accidental loss of teeth. This procedure’s advantage is that “it can be offered in young patients when the use of implants is not indicated because of the continuing alveolar growth.” (Andreason, et al, 2001, p.137(1) Trauma in the anterior mouth region is known to result in loss of incisor teeth. Incisor teeth can be replaced with transplanted premolars. Most suitable are the mandibular first and second premolars due to the anatomy of their root however, when the first mandibular premolars are not available the maxillary second premolar is appropriate for use. The maxillary first premolar has been found to be non-optional as a graft due to the divergent root anatomy of this tooth.
Andreason et al (2001) reports that the harvesting of the tooth germ ‘to be used as a donor tooth is the same for transplantation to anterior regions as it is for transplantation to agenesis sites.” (p.138; (1) The surgical preparation of the recipient site is reported as an open procedure with temporary removal of the “labial bone plate with subsequent repositioning of the bond after accommodation of the graft.” (Andreason, et al, 2001, p.138(1) It is reported that the transplanted tooth should be placed in infraposition, and a 0.2 steel wire should be placed over the crown of the transplant tooth and fastened around the neck of adjacent teeth.” (Andreason, et al, 2001, p.138(1)
Post-Operative Care
It is reported that this serve to “prevent the transplanted tooth from undergoing premature eruption.” (Andreason, et al, 2001, p.138(1) After four weeks, the teeth should experience stabilization in the new position and the splint can then be restored. The tooth can be restored after about four months however it is important that the lingual enamel be removed to ensure proper occlusion. (Andreason, et al, 2001, paraphrased) Dentin should optimally not be exposed however, if it cannot be avoided us of a dentinal bonding procedure is recommended. Experiential knowledge reports that transplanted teeth are likely to develop pulp necrosis if bacterial access to dentin formed occurs after transplantation because of the many vascular inclusions that are found in the secondary dentin. There can be restoration of the transplanted teeth with “composite or porcelain laminates.” (Andreason, et al, 2001, p.138(1)
Pulp Vitality
The work of Zhang and Yelick (2010) (20) reports that pulp vitality is critically important for the tooth viability as it makes provision of nutrition and act as a biosensor for detection of pathogenic stimuli.” Root canal treatment is one of the most often used techniques and is a procedure used for removal of contaminated or injured dental tissue, refilling and sealing off the void that has resulted with synthetic material to eliminate contamination in the future. Dentin is one of the primary mineralized tissue components of teeth and is reported as a tissue that is hard with “dentinal tubules penetrating throughout the entire thickness.” (Zhang and Yelick, 2010, p.1(20) The primary function of pulp is the production of dentin and this includes primary dentin during earth tooth development as well as secondary dentin produced throughout the lifespan of the individual and tertiary dentin under pathogenic stimuli. (Zhang and Yelick, 2010, p.1(20) When dental pulp is injured it has only a limited capacity for self-healing.
Previous Study Findings
Three long-term studies of transplants to the anterior region are reported with all of them reporting results that are favorable in the long-term. (Andreason, et al, 2001, paraphrased) The advantages of autotransplantation over implants includes that there is no bone induction in implants and implants require creation of a gingival papilla if possible. Implants require three-dimensional bone support and eruption is not a possibility. Furthermore it is not possible to move implants orthodontically and implants are limited to adults with debatable cost efficiency. Autotransplanted teeth however induce bone and induce a gingival papilla and there is not a requirement of bone support. Eruption is possible and autotransplanted teeth can be moved orthodontically with no requirements related to age of the individual. Finally autotransplanted teeth have high cost efficiency. (Andreason, et al, 2001, p. 150(1)
Complete Healing – Measure of Success
Complete healing is the measure for success in autotransplantation of teeth in addition to ongoing function and maintenance of a “health tooth0alevolar complex.’ (Andreason, et al, 2001, p.152(1) In the instance of transplanted teeth that are not completely developed the measure for success is stated to be “healing of the periodontal ligament without progressive root resorption, gingival healing, dental pulp, continued root formation, and normal alveolar bone.” Andreason, et al, 2001, p.152(1) In developed mature teeth the measure for success is stated as “gingival, periodontal ligament and bone healing.” (Andreason, et al, 2001, p.152(1) It is reported that the pulp could not be anticipated to revascularize and indication is always for root canal treatment. (Andreason, et al, 2001, paraphrased)
Radiographic Evidence of Success
The evidence of success measured radiographically includes:
(1) normal width of periodontal ligament space around the autotransplanted tooth;
(2) no evidence of progressive root resorption; and
(3) a radiopaque line on the side of the alveolar bone (lamina dura). (Andreason, et al, 2001, p.152(1)
Clinical Evidence of Success
Reported as clinical evidence of success is the following measures:
(1) Tooth mobility within normal limits;
(2) normal percussion sound;
(3) no evidence of loss attachment or no formation of pocket;
(4) no evidence of inflammation;
(5) no patient discomfort; and
(6) normal tooth function. (Andreason, et al, 2001, p. 152(1)
Histological Evidence of Success
Histological evidence of autotransplantation success is reported to be related mainly to demonstrating that the “restored periodontal ligament fibers are aligned perpendicular to the root and alveolar bone.” (Andreason, et al, 2001, p.152(1) In the case where the fibers are aligned “parallel to the root and bone then the case is not successful even in the case of clinical and radiographic evidence indicating healing. It is not possible to histologically evaluate clinical cases unless the tooth is extracted following failure. Also noted as controversial is uncertain clinical and radiographic evidence and the question remains whether these types of results should be deemed successful.
Evidence of Failure
Evidence of failure is reported to include:
(1) evidence of progressive root resorption; and
(2) evidence of no attachment gain or progressive attachment loss. (Andreason, et al, 2001, p.155(1)
Survival Rate of Autotransplantation
The reported survival rate of autotransplantation of teeth in the nonextraction site is stated at approximately 77% and the success rate is stated at approximately 60%. (Andreason, et al, 2001, p. 156(1) According to Andreason et al (2001) autotransplantation is more prone to success where the “donor tooth is transplanted to an extraction site with periodontal ligament attachment still present in the extraction socket.” (p.157(1)
Andreason et al (2001) reports that it is difficult through a review of the literature to attempt to determine the success rate of autotransplantation however, the results once extrapolated from the rates of periodontal ligament healing shows that the periodontal ligament of developing teeth heals more quickly than that of developed teeth and this results in survival success rates of developing teeth being higher than those of developed teeth. In addition, the root shape affects the predictability of the prognosis for premolar autotransplantation, which is best, and the worst for canine autotransplantation.
Primary Success Factor
The primary factor for success is reported in the work of Andreason et al (2001) to be that of “vital periodontal ligament attachment to the autotransplanted tooth and that the tooth continues to be functional.” (Andreason, et al, 2001) Necrosis or mechanical loss of the periodontal ligament leads to root resorption (ankylosis or inflammatory resorption) or epithelial downgrowth leading to failure. (Andreason, et al, 2001, p.161(1)
Root shape is stated to impact success in two ways:
(1) degree of extraction difficulty; and
(2) shape match between transplanted tooth and donor site. (Andreason, et al, 2001, p. 163(1)
Teeth with multiple roots and roots with excessive cementum and curved roots that might involve periodontal ligament injury or partial root fracture during extraction are all potential problems. It is reported that it is impossible at times to extract these teeth without inflicting such damage that they are of no use. Also difficult to match to the donor site is a multiple-root tooth with short root trunk or a single root tooth that is concave around the cervical area. (Andreason, et al, 2001, paraphrased) A functioning tooth has normal, functioning periodontal ligament attachment covering the root and nonfunctioning teeth such as those, which are impacted and chosen as the donor tooth result in less than ideal prognosis since there is the chance that there is inadequate periodontal ligament for development of a functioning attachment in the new site.
Factors Affecting Success Rates
Maturing of root structure is noted by Dr. Andresen and Dr. Schwartz to affect the success rates of autotransplantation. Success rates are lowered in cases in which autotransplantation is conducted to nonextraction sites in patients who are older resulting in less than ideal prognosis of autotransplantation of mature teeth and a better prognosis for autotransplantation of developing teeth. High success rates however are noted in the autotransplantation of mature teeth to extraction sites meaning that the success rate cannot be based on the root maturity solely and factors influencing the success rates in terms or the shape of the root or the mature teeth length must be considered. It is reported that the “longer and more complicated” the shape of roots the more chance that there will be injury to the periodontal ligament during extraction of the tooth. In the case of vital or nonvital pulp tissue it is unclear if root canal therapy has any impact on the autotransplantation success. (Andreason, et al, 2001(2)
It is reported that not much difference exits in gingival or periodontal ligament healing between autotransplanted teeth that have not undergone root canal therapy and those that have. In the case of developing teeth however, extraction is easy in young patients resulting in a higher level of healing and healing is generally quicker. Stated as a concern of vital tooth autotransplantation is the presence of pulpal infection, which affects the prognosis, and a concern of root-filled teeth is related to the chance of secondary caries and fracture of the root. (Andreason, et al, 2001, paraphrased)
Evidence exists that replanted teeth may be more likely to develop resorption in the case where they have been splinted rigidly for an extended time. This consideration is important however, the stabilization of transplanted teeth until attachment has occurred is equally important as the goal is stated as achieving functional attachment.
The work of Marques-Ferreira, et al (2011) reports a study that assessed the pulp survival that occurs in transplants of autologous teeth through comparison of two surgical techniques: (1) conventional technique; and (2) an alternative technique. The study group consisted of 26 patients involving 28 transplanted teeth to recipient sockets prepared mechanically. Only two transplanted teeth were reported as being lost “due persistent apical periodontitis and one transplanted patient with open apex missed the treatment.” (Marques-Ferreira, et al, 2011)
It is reported in the teeth with pulp there was a need to perform root canal therapy in 9 teeth and in teeth with closed apex, root canal treatment was needed in 73% of the teeth. There was not statistical difference stated among closed apex and root canal therapy and only 8% of the teeth with open apex required root canal treatment with an overall success rate stated at 98%. Conclusions stated is that while it is not a frequent procedure “autotransplanted teeth, performed with appropriate surgical care had a good prognosis, and can render a very useful service to the patients.” (Marques-Ferreira, et al, 2011, p. 984(9)
The work of Park, Tai and Hayashi (2011) states autotransplantation is defined “as the transplantation of embedded, impacted or erupted teeth from one site into extraction sites or surgically prepared sockets in the same person. Autotransplantation has been used to replace missing teeth and teeth of poor prognosis.” (p. 129(12) The etiology of tooth agenesis is reported as largely unknown. The work of Vastardis is reported to have presented supporting evidence of a genetic etiology for tooth agenesis and reported that the teeth most commonly absent are “third molars followed by mandibular second premolars.” (cited in Park, Tai, and Hayashi, 2011, p.129(12) There are stated to be reports of associations of tooth agenesis and other congenital tooth anomalies to certain malocclusions and that the treatment plan for missing teeth cases Should be based on a comprehensive evaluation of the age, occlusion and space requirements of the patients as well as the size and shape of the adjacent teeth.” (Park, Tai, and Hayashi, 2011, p.129) If extraction has been planned in the maxillary for the correction of crowing or reduction of an overjet, a maxillary premolar may be transplanted to the second premolar site in the mandible.” (Park, Tai, and Hayashi, 2011, p.129(12)
In the majority of cases, the tooth or teeth to be extracted due to caries or periodontal disease are the first molars and it is reported that in this case that transplantation of third molars to the first molar site may be considered. (Park, Tai, and Hayashi, 2011, paraphrased) Autotransplantation is reported to provide “a simplified and faster treatment option for patients with ectopically positioned teeth.” (Park, Tai, and Hayashi, 2011, p.129(12) The sequence stated for autotransplantation includes “clinical and radiographic examination, diagnosis, treatment planning, a surgical procedure, possible endontic treatment, restorative treatment and maintenance.” (Park, Tai, and Hayashi, 2011, p. 130(12) Timing of the extraction of the tooth from the recipient site should undergo careful determination and when extraction is prior to the transplantation date, transplantation should be performed as quickly as possible. (Park, Tai, and Hayashi, 2011, paraphrased) Indications for transplantation are stated as follows:
When donor teeth are maxillary premolars the recipient sites or agenesis sites (the mandibular second premolars) with indications and prognosis stated as follows: “If maxillary premolars are to be extracted for orthodontic reason, they can be transplanted to the mandibular second premolar site. The high predictability of this procedure and its dependence on the state of root formation has been confirmed in several long-term studies.” (Park, Tai, and Hayashi, 2011, p. 131(12)
Premolars – donor teeth by first choice are mandibular first and second premolars because of their root anatomy, and the second choice would be the maxillary second premolar. The maxillary first premolar is not recommended due to its divergent root. The recipient site is stated as the maxillary anterior region. Indications and prognosis are stated as follows: ‘Could be considered in children with accidental teeth loss where implants are contradicted because of continued alveolar bone growth. The transplanted teeth can be restored with composite or porcelain laminates. Long-term studies of transplants to the anterior region demonstrated favorable long-term results.” (Park, Tai, and Hayashi, 2011, p.131(12)
Third molar donor teeth are stated as the first or second molars to recipient sites and agenesis sites or the second premolar region. Indications and prognosis are stated as follows: Potential for severe dental caries, endodontic problems, or juvenile periodontitis. The donor should be removed from the socket atraumatically. Making an accurate evaluation of the mesiodistal distance of the recipient site is important. The outcome of third molar transplantation seems less favorable than premolar transplantations; however, 75% of transplants have been successful over a long period of time.” (Park, Tai, and Hayashi, 2011, p.131(12)
Treatment options for congenitally missing teeth include:
(1) extraction of primary teeth, which allows adjacent teeth to close the space spontaneously;
(2) retention of primary teeth if they are not anklyosed;
(3) extraction of deciduous teeth and closure of the space orthodontically;
(4) replacement of teeth with implants when facial growth is completed;
(5) the placement of fixed metal or ceramic prostheses;
(6) the placement or removable partial dentures; or
(7) the use of resin-bonded fixed bridges. (Park, Tai, and Hayashi, 2011(12)
Retaining primary teeth is stated as a possible option for aplasia. (Park, Tai, and Hayashi, 2011, p.132(12)
The work of Sharma, et al (2010) reports a study involving a 10 year old boy in which the impaction of a developing maxillary second premolar was detected in routine othorpentograph conducted at regular intervals for serial extraction. The patient did not claim discomfort and intra-oral examination revealed that “all first premolar extracted and all permanent teeth were erupting well except for all retained second deciduous molars.” (Sharma, et al, 2010(15) However, there was a prominent bulge on the left palate detected in primary maxillary left second molar region. The bulge is reported as being “hard, non-tender, and non-inflammatory, indicating palatal impaction of maxillary left second premolar.” (Sharma, et al, 2010(15) The study reports that autotransplantation during mixed dentition period offer advantages of partial root development of premolars. Tanaka et al and Kvint et al provided descriptions of premolar sand permanent canines to the recipient site of retained deciduous teeth with a success rate at 100% in a four year follow up for premolars and 84$ for canines when recipient sites were in maxilla.” (Sharma, et al, 2010(15) Slagsvold and Bjercke states that if integrity of epithelial sheath in the donor tooth is maintained that genetics might serve to control root growth and root formation that is adequate could be secured. The work of Tsukibosh states an 82% success rate “when premolars were transplanted into the fresh socket while it was 60% when transplanted to artificially formed socket.” (Sharma, et al, 2010(15)
The work of Park, Tai and Hayashi (2011) report “Autotransplantation of teeth offers a new treatment option for some clinical situations. It permits tooth movement to distant or opposite sides of the same dental arch, as well as to the opposite jaw. Furthermore, transplantation offers other potential benefits such as bone induction and the reestablishment of a normal alveolar process in addition to tooth replacement. Even if the transplant fails later, there is an intact recipient area that could be used for an implant. A prerequisite for this method, however, is a thorough knowledge of the factors that influence the long-term success rate. If done properly, this method may supplement and or be used as a viable treatment option in present day clinical practice.” (p.133-34(12)
Likewise the work of Miranda, et al (2009) reports that autotransplantation is a method with “optimum, indication for a 10-year old child because alveolar growth is not yet complete contraindicating implants or fixed prosthetics. Furthermore, the transplant establishes a functional tooth unit which allows the development of alveolar bone.” (p.48(10) These findings are echoed in the work of Andreason, Andersson, and Tsukiboshi (2007(1) and Toledo-Filho, Longo-Filho, and Marzollar (2009(18).
The work of Cho and Lee (2007) reports a study of a patient, a 12-year old boy referred to management of an impacted mandibular right first premolar. The boy was reported as in permanent dentitation with the right first premolar and all third molars unerupted” His mandibular and permanent molars are reported to have been extracted by his referring dentist at the age of 11 years and 11 months of age. At that time the orthopantomogram was taken and revealed “unerupted premaxillary mesiodens and a supplemental premolar impacted with the mandibular right first premolar. Crown formation on the supplemental premolar was complete. The parents agreed that early removal of the supplemental premolar would be needed to facilitate eruption of the impacted first premolar. “(Cho and Lee, 2007(3)
The parents however, stated a preference not to extract the mesiodens as it was deeply seated and not associated with pathosis.” (Cho and Lee, 2007(3) Reported is the extraction of the first molars for treatment options of the spaces. Further orthodontic space closure was declined by the parents and patient due to the treatment costs not being covered by the public dental service in which the patient was enrolled. It is reported that proposed was “Autotransplantation of the supplemental premolar to the mandibular right molar region” as an option that was, less than desirable, still to be an option.
The autotransplantation involved local anesthesia, followed by raising of mucoperiosteal flaps in the mandibular right first premolar and first moral areas. Partial healing of the first molar socket is reported and the recipient site prepared “…with a surgical round bur cooled with sterile saline. The supplemental premolar was carefully extracted, keeping the radicular part intact and untouched, and was transplanted to the first molar area without extraoral storage.” (Cho and Lee, 2007(3) Black silk sutures were used in stabilizing the transplant and for wound closure. The patient was given chlorhexidine rinse and amoxicillin for one week and then reviewed at week 1, month 1, 3 months, and every six months. Reported are continued growth of root and “no clinical or radiographic sign of resorption.” (Cho and Lee, 2007(3)
Discussion
The findings in this study have demonstrated that restorative dentistry can be arduous with the pediatric patient when congenitally missing teeth create edentulous spaces. Autogenous tooth transplantation is an appropriate method for use in children with developing teeth and is a procedure with a high success rate. In the cases reviewed in this study, it has been demonstrated that autogenous transplantation of teeth in children is an effective method and one that is highly successful under the right conditions.
In the case study reported in this work in writing the proper procedures were followed and the tooth was stabilized for eight weeks. The literature reviewed in this work has demonstrated that transplantation in children with accidental tooth loss is a procedure that should be considered and one that provides advantages in young patients where implants are not appropriate for use. The benefits of the use of this procedure in pediatric patients are clearly indicated in the study and precise measures for success have been stated to give the practitioner in this procedure when used in treating children.
Bibliography
(1) Andreasen JO, Andersson L & Tsukiboshi M. 2007. Autotransplantation of teeth to anterior region. In: Andreasen JO, Andersson L & Andreasen FM. Textbook and color atlas of traumatic injuries to the teeth. Wiley-Blackwell, 740–59.
(2) Clokie, Cameron; Yau, Deirdre M., and Chano, Laura (2001) Autogenous Tooth Transplantation: An Alternative to Dental Implant Placement. J Can Dent Assoc 2001; 67-92-6.
(3) Cho, SY and Lee, C (2001) Autotransplantation of A Supplemental Premolar: A Case Report. Clinical Practice. June 2007. Vol. 73 No. 5.
(4) Cohen AS, Shen TC, Pogrel MA. Transplanting teeth successfully: autografts and allografts that work. JADA 1995; 126(4):481-5
(5) Kahnberg KE. Autotransplantation of teeth: indications for transplantation with a follow-up of 51 cases. Int J Oral Maxillofac Surg 1987; 16(5):577-85.
(6) Kugelberg R, Tegsjo U, Malmgren O. Autotransplantation of 45 teeth to the upper incisor region in adolescents. Swed Dent J 1994; 18(5):165-72
(7) Kvint, S, et al (2010) Autotransplantation of Teeth in 215 Patients. Angle Orthod 80:446-451.
(8) Lundberg T, Isaksson S. A clinical follow-up study of 278 autotransplanted teeth. Br J Oral Maxillofac Surg 1996; 34(2):181-5.
(9) Marques-Ferreira, M. et al (2011) Autogenous Tooth Transplantation: Evaluation of Pulp Tissue Regeneration. Medical Oral Patol Oral Cir Buccal 2011, Nov 1;16(7).
(10) Miranda. RB (2009) Autogenous Tooth Transplantation: A Case Report. Brazilian Journal of Dental Traumatology. 1(2) 45-49.
(11) Northway WM, Konigsberg S. Autogenic tooth transplantation: the “state of the art”. Am J Orthod 1980; 77(2):146-62.
(12) Park, JH, Tai, K, and Hayashi, D (2011) Tooth Transplantation as a Treatment Option: A Review. J. Clin. Pediatr Dent 35(2): 129-136, 2011.
(13) Schwartz O, Bergmann P, Klausen B. Autotransplantation of human teeth: a life-table analysis of prognostic factors. Int J Oral Surg 1985; 14(3):245-58
(14) Schwartz, O., Bergmann, P. and Kilaussen, B. (19850 Resorption of Autotransplanted Human Teeth: A Retrospective Study of 2981 Transplantation over a period of maxillary left second premolar years. Int. Endon J 18: 119-131.
(15) Sharma, DS, et al (2011) Autotransplantation of an Impacted Second Premolar in its Predecessor’s Socket with the Novel Use of Modern Imaging System: A Case Report with 18 months Follow Up. Trauma & Treatment. 2011 1.1.
(16) Slagsvold, O. and Bjerck, B. (1974) Autotransplantation of Teeth, Predictable Success. Dent Traumatol 18: 157-180.
(17) Tanaka, T. et al (2008) Autotransplantation of 28 premolar donor teeth in 24 orthodontic patients. Angle Orthod 78: 12-19.
(18) Toledo-Filho JL, Longo-Filho JS & Marzolla C. 2009. Incisive transplantation – a retrospective study. Revista ATO [on line] 2009 [cited 2009 Mai 15].
(19) Tsukiboshi, J. (2002) Autotransplantation of Teeth: predictable success. Dental Traumatol. 18: 157-180.
(20) Zhang, W. and Yelick, PC (2010) Vital Pulp Therapy – Current Progress of Dental Pulp Regeneration and Revascularization. International Journal of Dentistry. Vol. 2010.
Appendix ‘A’
Figure 1 – A Pre-surgical Panorex Showing Retained Dentition at Lower Central Incisor Site
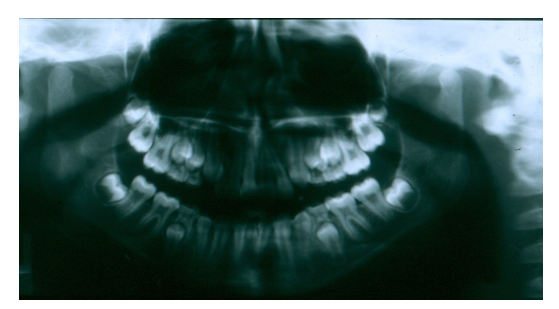
Figure 2 – Recipient Site – Presurgical Photograph Mandibular Central Primary Incisors

Figure 3 – Supernumerary Transplant Donor From Maxillary Left Lateral Site

Figure 4 – Maxillary Supernumerary Tooth Inverted and Transplanted to Mandibular Central Incisor Site

Figure 5 – Radiograph Follow-up of Transplanted Supernumerary
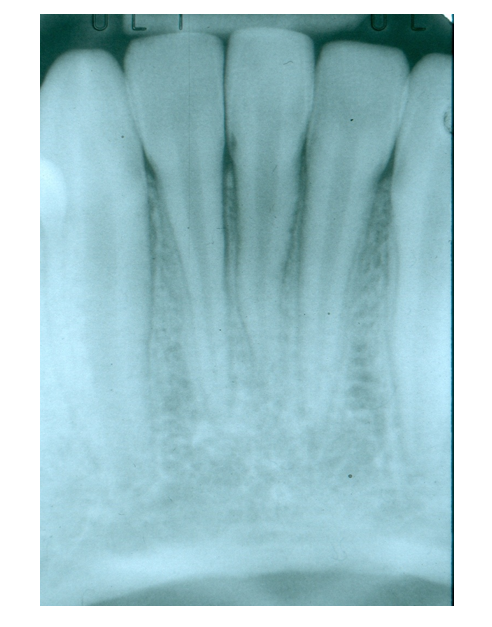
Figure 6 – 6-month post-transplant Recipient Site Healing

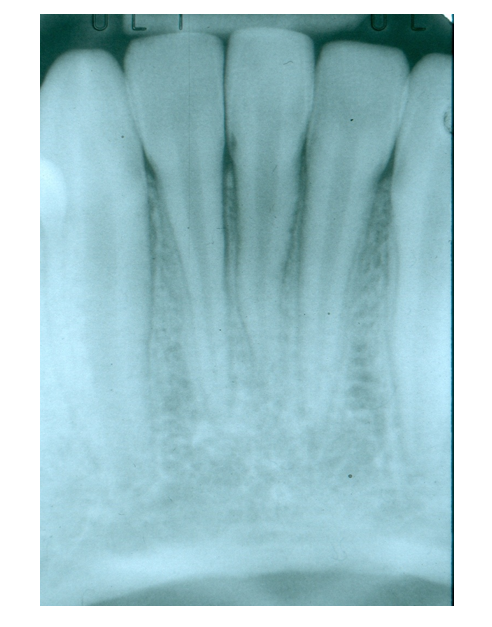
Figure 7 – 5-year follow-up of Transplanted Supernumerary at Mandibular Central Site

Figure 8 – 5-year follow-up of Transplanted Supernumerary at Mandibular Central Site

Time is precious
don’t waste it!

Plagiarism-free
guarantee

Privacy
guarantee

Secure
checkout

Money back
guarantee






