Ventilator Acquired Pneumonia, Capstone Project Example
Abstract
Intensive care units (ICU) serve as the site where gravely ill individuals recuperate from their perilous afflictions. However, it is in this very “care” unit where seemingly careless regard for the patients accounts for the “second most common nosocomial infection in critically ill patients.” Ventilator-associated pneumonia (VAP) is this disease. VAP is a lung infection that is caused by prolonged (two days or more) reliance on a ventilation machine (Koenig, & Truwit, 2006). If the ventilation tubes that provide oxygen to the patient become contaminated with pathogens, then VAP develops when these organisms find their way to the patient’s pulmonary organs (Ventilator-Associated Pneumonia (VAP), 2012). Also referred to as hospital-acquired pneumonia (HAP), this preventable sickness has been known to increase hospital stay and hospital costs—the former by at least a week, the latter by at least $40,000 per patient (Amanullah, & Posner). Ventilator-associated pneumonia occurs in 28% of mechanically ventilated patients with a mortality rate ranging from 27-76%—increasing if “appropriate and adequately dosed antibiotic therapy” is not rapidly applied (Amanullah, & Posner.
Acknowledgements
I would like to take this opportunity first and foremost to give thanks to my God, without Him the requirements to complete this project would be futile. This journey would not have been possible without the support of my family, professors, mentors, and friends. I give special thanks to my husband and three children who supported me every inch of the journey and to my mom and dad, sisters and brothers my pastor and family who inspired me. Their optimism drives me every day; they support me in every aspect. I would like to express my deepest appreciation to my Capstone Chair and mentor; Dr. Rivers who have provided much direction for me when I was totally lost. You have given your time, expertise, untiring support and guidance throughout my journey. Thanks so much for all the support that you gave me, the endless e-mails back and forth, clarification of misunderstood information, your prompt and professional responses to my questions, your motivation, and the care and concern you have shown me throughout the course. Last but definitely not least, I must thank my course mentor. Rovina Billingslea simply the best. You have motivated me, my e-mails and phone calls were always answered promptly, you were there to guide me through, and it is greatly appreciated. The journey was long and tedious, there were ups and downs but through it all, I made it with all of your support. Thanks to all.
Chapter 1: Introduction to the Problem
Background and Overview
Intensive care units (ICU) were the site where gravely ill individuals recuperated from their perilous afflictions. However, it is in this very “care” unit where seemingly careless regard for the patients accounted for the “second most common nosocomial infection in critically ill patients” (Koenig & Truwit, 2006, p. 637), better known as ventilator-associated pneumonia (VAP). Most cases of VAP have developed as a direct result of clinic practices. Therefore, it was important to understand the progression of the illness.
According to Koenig and Truwitt, VAP is a lung infection caused by prolonged (two days or more) reliance on a ventilation machine and is known as a “healthcare-associated infection” (Center for Disease Control and Prevention (CDC), 2012, Title). The CDC stated VAP developed when the ventilation tubes providing oxygen to the patient became contaminated with pathogens and found their way to the patient’s pulmonary organs. Often the cause of 90% of hospital-acquired infections, VAP took place within 48 hours of intubation (Lau, O’Keefe-McCarthy, & Santiago, 2008). Ventilator-associated pneumonia is usually suspected when the individual develops a new or progressive infiltrate on chest radiograph, leukocytosis, and purulent tracheobronchial secretions. Unfortunately, and unlike the criteria for community-acquired pneumonia, accepted clinical criteria for pneumonia were of limited diagnostic value in definitively establishing the presence of VAP (Tablan, Anderson, Besser, Bridges, & Hajjeh, 2004). In most cases, VAP was a preventable disease, and its occurrence in preventable cases has potentially severe clinical and economic losses for the patient, the hospital, and the healthcare system.
The clinical consequences of preventable VAP occurrences were substantial. When clinical consequences were realized, they most often translate into economic costs and needless loss of life. A type of hospital-acquired pneumonia (HAP), this preventable sickness has b increased hospital stay and hospital costs—the former by at least a week, the latter by at least $40,000 per patient, Amanullah (2013) conveyed. As Amanullah (2013) stated, VAP occurs in 28% of mechanically ventilated patients with a mortality rate ranging from 27-76%—increasing as it is not immediately recognized and treated.
In addition, having had to treat a case of preventable VAP produced other consequences that result in loss of life. “Increasing drug-resistance rates among gram-negative pathogens that frequently cause ventilator-associated pneumonia” according to Amin (2009, p. S36) have resulted in increased healthcare cost as well as longer hospitalization for patients and higher mortality rates in healthcare settings, explained Amin.
According to Vima Medical (2011), despite the fact that the medical field has recognized the importance of having a protocol to follow and implement in the prevention of VAP, these programs have not been applied with consistency:
The key components of the Ventilator Bundle are: Elevation of the Head of the Bed (HOB >30°), Daily ‘Sedation Vacations’ and Assessment of Readiness to Extubate, Peptic Ulcer Disease Prophylaxis, Deep Venous Thrombosis Prophylaxis and Daily Oral Care with Chlorhexidine. (Vima Medical, para. 4).
Mechanical intubation inhibited the patient’s ability to yield to his or her cough reflexes and hindered the effective eviction of built-up mucus that can seep infectious bacteria into the lungs, according to Lau et al. (2008). The result of mechanical intubation was often the inability of the patient to yield to his or her cough reflexes, which hindered the effective eviction of built-up mucus that can seep infectious bacteria into the lungs, according to Lau et al. (2008). Recognized as a continuous dilemma for critical care nurses, VAP was often approached by the “use [of] current evidence-based strategies to decrease its incidence and prevalence” (Lau et al., 2008, p. 193).
In the prevention of VAP, many educational training programs have been introduced to train nurses and healthcare workers in practices that are thought to prevent VAP. People opposed to these training programs claim the typical points of training are not validated in research, and might even be detrimental to the patient (O’Grady, Murray, & Ames, 2012). If groups of healthcare workers question the practices conventionally thought to prevent VAP, there isn’t any motivation to follow them if the practices are called into question. Therefore, it is the intention of this study to test if the Association for Professionals in Infection Control and Epidemiology’s (APIC) protocol is effective in lowering the cases of VAP in an ICU setting.
Investigation into the background and overview of VAP revealed many occurrences of VAP arise from a failure to follow infection prevention protocol. Maselli (2011) described certain causes of VAP as inherent; risk factors patients arrive with, including depressed immune systems due to severe illness such as cancer and HIV, and external factors, such as a failure of hospital staff to sanitize their hands after each patient. This study concentrated upon how adherence to a consistent protocol reduced the number of preventable cases of VAP. The problem statement and the rationale and significance of the study explained the importance of finding ways to lower the amount of incidences of preventable VAP.
Problem Statement
As healthcare professionals have been extensively trained to ensure that patients heal rather than worsen after a stay at the hospital, the ill afflicted have trusted them with their lives. Ventilator-associated pneumonia (VAP) was an ailment a dependent patient acquires when the nurses and Respiratory therapists who are responsible for their recovery have not sufficiently abided by the protocols to prevent infection. Whilst losing the trust of the patient and his or her family, the healthcare provider responsible for the full manifestation of the preventable disease also costs his or her place of employment a fraction of its credibility. For the sake of the betterment of the medicinal field, the researcher chose this topic as a way to raise awareness about the importance of proper preventative procedures regarding VAP so that patients would no longer have to suffer because of incompetence and inconsistency in their healthcare giver’s craft.
Rationale and Significance of the Study
The importance of this project to the researcher’s discipline resides in the name of improvement. The medicinal field was always in need of enhancement; if not, VAP would not be a detrimental factor that plagues the hospital setting’s existence and reliability. This project sought to discover the most efficient way of reducing if not completely eliminating this infection (and others possibly acquired in a hospital setting) through the development of a structured regimen that sought to discipline healthcare givers into wholly complying with hospital standards without having to face debasing consequences on their and the hospital’s behalves.
Purpose Statement
The purpose of this study was to assess the success of using a protocol, such as the procedures and documentation proposed by The Association for Professionals in Infection Control and Epidemiology (APIC) in decreasing the amount of reported cases of VAP within an ICU setting.
Research Question(s)
This research study sought to utilize a quantitative case study method. The study’s research questions are detailed below:
What teaching strategies were implemented in the Intensive Care Unit to care for patients that were intubated?
How did the implementation of VAP teaching strategies in the ICU compare in terms of learning outcomes and performance to traditional classroom programs?
What were some possible solutions for developing a more effective practice to insure VAP prevention coursework and training programs for future nurses? What would be the experience of Vap if the ICU did not have VAP prevention programs?
This experiment did not involve any form of human experimentation or testing.
This study did not include children (individuals under the age of 18) among the study’s respondents.
In order to minimize any risk to the study’s respondents all participation was completely confidential with the researcher being the only individual to have access to identifying information. Furthermore, after five years, all records pertaining to study respondents will be destroyed by members of the department and the researcher. Finally, This study’s survey respondents did not include any members of a vulnerable population participation in the study itself was completely voluntary and could be withdrawn at any time during the study, including requesting the final results to omit a respondent’s information .
The researcher ensured complete confidentiality by assembling the sample frame and the sample pool independently. Additionally, the final record of survey respondents was placed in a sealed envelope or file and retained only for a period of five years after which it will be destroyed
Hypothesis(es)
The researcher hypothesized that if the nurses comply with the health precautions and the procedures in place, then the occurrences of VAP within the hospital setting would drastically decline because of improving adherence to VAP protocols. Due to the fact that VAP is a preventable disease, if the preventions were executed, then the disease would be annihilated. This rationale was the foundation for the following research question:
Was establishing and implementing APIC’s VAP prevention protocol an effective producer of lower occurrences of VAP in intensive care units?
following are the null and alternate hypotheses for the study. The null hypothesis reflected no effect once the VAP prevention program is established. If the alternate hypothesis was proven, the establishment of the VAP prevention program was effective in reducing the incidences of VAP in an ICU setting. The independent variable was the APIC training and guidelines. The dependent variable was the number of VAP related illnesses and deaths in an ICU setting.
H0: The implementation of the APIC training and guidelines did not decrease the occurrences of VAP in an ICU setting.
H1: The implementation of the APIC training and guidelines did decrease the occurrences of VAP in an ICU setting.
Definition of Term
Summary
In chapter one, the overview and background of the problem of VAP was presented. The problem statement, rationale of the study, purpose, and hypotheses were presented. Terms that will be used throughout the paper were defined.
Chapter 2 presented the literature review. After a brief introduction, the two types of factors thought to contribute to the progression of VAP were explained. Best practices to prevent VAP progression were also described in general, followed by a detailed description of APIC’s VAP prevention protocol and the summary and conclusion for the chapter.
Chapter 2: Literature Review
Introduction
The literature review consisted of various studies that that were done on implementation of an education initiative use of evidence-based practice and guideline recommendations. The literature review explained the preventable and unpreventable factors that contributed directly to the development of VAP and best practices in the prevention of VAP. Anticipatory measures and best practices were vital characteristics of nursing care for patients who receive mechanical ventilation.
Causes and Factors of VAP
A review of the literature revealed two types of factors that were found to contribute to the occurrence of VAP. Maselli (2011) found there were some factors that could be controlled for within a healthcare setting, and some factors were inherent in the condition of the patient.
Inherent Patient Risk Factors
Some patients were naturally at higher risk to develop VAP than other patients. Some factors, conveyed Maselli (2011), contributed to the development of VAP that outside the control of hospital staff if the patient is above the age of 60 and male, if the patient had an upper respiratory infection, multiple organ dysfunction syndrome (MODS), coma, chronic bronchitis or emphysema, a tracheotomy, multiple intubations, injuries to the cranium or brain, and neurosurgery. Other factors that put a patient at risk for infection were as follows: “Patient has received hemodialysis, wound, or infusion therapy as an outpatient; patient was previously hospitalized for at least 3 days within the past 90 days prior to current admission; or the patient is immunocompromised due to underlying disease or therapy (HIV, chemotherapy” (APIC, 2009, p. 10).
However, there were many factors that contributed to the development of VAP that healthcare workers could control to reduce the incidences of VAP within the health care setting, if not all cases, despite inherent factors. The following section described hospital-associated causes of VAP.
Hospital-Associated Causes of VAP
There was more motivation than ever to reduce HAIs from occurring. Insurance companies ceased payments on “preventable” diseases, basically diseases that were acquired in hospitals, stated Paciella (2009). The costs for these diseases are directly out of the pocket of the hospital, because the hospital did not receive reimbursement for treating the illness and the hospital was not allowed to charge the patient for the care (Paciella, 2009).
Research established that many causes of VAP were caused by factors that were directly linked with the care of the intubated patient. There were several possible contributing factors for the development of VAP as Pitett (2003) outlined. Hand hygiene was considered the primary measure that reduced the transmission of nosocomial pathogens. Noncompliance with hand hygiene remained a major problem in hospitals. Due to poor hygiene, more and more patients were being exposed to various types of nosocomial pathogens and infections. These infections range from a common cold to life threatening illnesses. Following recent improvements in our understanding of the epidemiology of hand hygiene compliance, new approaches have been suggested. Guidelines for hand hygiene have been revisited and should improve the standards and practice in healthcare settings.
Another source of infection was the conditions created by the tracheal tube. John Hopkins Medicine (n. d.) explained when a breath of air is inhaled; it is naturally heated, cleansed, and moistened. A tracheal tube circumvented the natural breathing process, and the forced oxygen is colder, lacks moisture, and not as sterile. The body creates an increased amount of mucus. The tracheostomy tube is suctioned to remove mucus from the tube and trachea to allow for easier breathing and mitigate the chances of pulmonary infections. Normally, a patient should be suctioned every 4 to 6 hours and as needed to reduce the risk of bacterial infections in the pulmonary tracheostomy. It is imperative patients are suctioned within the appropriate time periods set forth by the hospital to mitigate various pulmonary infections and reduced hospital cost.
Williams, Chan, and Kelly (2008) highlighted problems that can arise from improper head elevation: “Elevation of the head-of-bed (HOB) of intubated patients is an effective method for reducing rates of aspiration pneumonia.” (para. 9). Williams et al. expressed a patient elevated at less than a 30-degree angle is one of the leading preventable causes of contracting the illness. Williams et al. found if other non-modifiable risk factors are controlled within a study, such as advanced age, recently taking prescription antibiotics, and massive organ failure, as well as other modifiable contributions, such as hand washing and tracheal tube maintenance, head positioning was identifiable in its role in the development of VAP within 24 hours of intubation.
Maselli (2011) expressed healthcare workers can make a big difference in the reduction of VAP through factors associated with the direct care of the patient. These factors include maintenance of a head elevation position between the 30 and 45 degree angle, which decreases the amount of hydrogen, carbon dioxide, or methane collecting in the digestive system, “contamination of ventilator circuits, [and] frequent patient transfers and low pressure of the endotracheal tube (ETT) cuff” (Introduction, para. 2). Other hospital procedures shown to reduce incidences of VAP included consistent hand sanitation, adherence to reporting requirements for washing hands, and patient dental hygiene maintenance (if a certain protocol is not followed in teeth cleaning, bacterial contamination can take place).
However, various gaps existed between what was expected of healthcare workers to be practiced and what actual care patients received. The next section identified best practice, examined current health care practice, and evaluated compliance after an educational involvement. The best way to achieve the ambitions of this study was to utilize a comprehensive program that could help track progress and generate data for research.
In the APIC (2009) system for VAP prevention, there were some core concepts that drove the concepts behind best practices. The core concepts were discussed along with the APIC practices to demonstrate the features of the protocol.
Best Practices for the Prevention of VAP
In this section, The Association for Professionals in Infection Control and Epidemiology (APIC) were described in terms of their goals and their activities to understand their authority in the subject of infection prevention, followed by a description of their VAP prevention program and how its features aligned with best practice procedures.
APIC (n. d.). APIC described their association as a collective consensus of health care professionals such as nurses, emergency care workers, doctors, scientists, and “medical technicians who” (Para. 2):
Collected, analyzed, and interpreted health data in order to track infection trends, plan appropriate interventions, measure success, and report relevant data to public health agencies.
Established scientifically based infection prevention practices and collaborated with the healthcare team to assure implementation.
Worked to prevent healthcare-associated infections (HAIs) in healthcare facilities by isolating sources of infections and limiting their transmission.
Educated healthcare personnel and the public about infectious diseases and how to limit their spread. (APIC, n. d., para. 2)
Their role in policy-making and ties to Congress were noteworthy and influential, serving as a source of information for policy makers as they created legislation to ensure public safety (APIC, n. d., Public Policy and Advocacy). The following sections described the features of the APIC (2009) VAP prevention system that coincided with concepts behind best practices in nursing. These concepts aligned with widely accepted nursing research and projects that sought to improve current practices.
Evidence Based Practices (EBP). APIC (2009) stated their Guide to the Elimination of Ventilator-Associated Pneumonia is based upon EBPs. EBP is not just a buzzword. EBP is defined as “innovative interventions that are based on best practices as well as solid research-based evidence” (Majid, Foo, & Mokhtar, 2011, p. 229), and has become an increasingly integral part of the nursing field.
Evidence-based practice explores the empiric way of knowing, focusing on Methods of critically appraising and applying available data and research to understand and inform clinical decision-making better. Although it clearly is not the only way of knowing, evidence-based practice provided a way to frame and address questions about how to provide the best patient care. For the Purpose of this article, the following definition of evidence-based practice was selected: “the integration of best research evidence with clinical expertise, and patient values”. (Pipe, Wellik, Buchda, Hansen, & Martyn, 2005, p. 365)
Gap Analysis. Kempnich (2011) explained a gap analysis was used to analyze, then express current policies and nursing practices in order to find gaps between existing practices and best practices, gaps in knowledge, adherences to best practices, and gaps in patient outcomes (desired health outcomes versus present health outcomes). According to Devo (n. d.), gap analysis process began with a self-assessment. Then the self-assessment was compared to the standards usually provided from governmental organizations aiming to improve safety and adherence to regulations and standards. For this study, a gap analysis was used and was described in detail in the methodology section.
Learning as a Collaborative Effort.
According to Kempnich, (2011), collaboration as a team optimized learning efforts. The APIC bundle for VAP prevention utilized the concept of a team effort in training, education, practices, and prevention and expounded upon the collaborative effort, equal appreciation for respect, and team member responsibility..
Ensuring “Safe and Reliable Care” (Vanderbilt University Medical Center, n. d.).
Vanderbilt University Medical Center associated safe and reliable care with forming teams of qualified nurses who had mutual respect for their areas of expertise and skills to reduce hospital-acquired infections (HAI). The following standards were incorporated into the APIC bundle:
Consistently achieved and exceeded all of the publicly reported and internally developed core measures targets as well as complied with all regulatory standards
Reduced hospital acquired condition rates to be at or below the established target for all state and CMS reported conditions.
Supported the deployment and use of evidence based order sets and decision making where applicable.
Reduced the potential risk for known high-risk processes
The Role of the Hospital Administration.
Clarke and Donaldson (n. d.) and Vanderbilt University Medical Center (n. d.) agreed that the hospital administration molded the attitude, work culture, procedures, and safety measures within the healthcare setting. Employees took their cues from hospital administration. APIC accounted for the roles the hospital administration plays and strived to involve them by establishing reporting systems based on hardcore data for job fulfillment and unit goals department goals.
Capturing Relevant, Timely Data to Improve Patient Care.
As Clarke and Donaldson (n. d.) stated, “Clearly, capturing data about patient outcomes prospectively (i.e., as care is delivered) is the best option for obtaining precise, comprehensive, consistently collected data. This approach was the most challenging because of practical, ethical, and financial considerations” (p. 10). The APIC (2009) system had built into it data charts that helped to capture relevant data and tracked progress on keeping down infections in critical care units.
Providing a Uniform Training Protocol.
The Critical Care Nurse Training Standards Task Group (n. d.) cited the importance of having a standardized, evidence-based training protocol to educate ICU nurses and staff. The APIC system contained the elements one needs for adequate training. Adequate training, stated the Critical Care Nurse Training Standards Task Group (n. d.), started with providing standard and consistent guidelines and procedures on how to perform the duties necessary that fulfill the job of ICU nurse, which in turn adhered to standards that promoted patient safety.
Description of the Guide to the Elimination of Ventilator-Associated Pneumonia (APIC, 2009). Nurses played a large role in the care of patients. Since nurses were the ones that have the most contact with patients, they made the most difference in decreasing preventable incidences of VAP. Having a comprehensive program to follow and track results helped nurses in their practice and in the prevention of VAP.
Programs to prevent the occurrences of VAP had been created to encompass everything from direct patient care to documentation to keep track of the occurrences of VAP, adherence to protocols, and administrative tracking of all aspects of the program to reduce VAP and help nurses in their practice and care of ICU patients.
APIC (2009) offered a comprehensive program free of charge on their website. The program offered all the necessary paperwork for all departments within a hospital setting, which made the implementation of their program and the recording of the results after the program is instilled traceable, and generates data that can be used in course of research. APIC’s comprehensive program for the prevention of VAP includes nurse education and follow up in adherence to procedures. The aspects of this program are outlined below.
APIC (2009) recommends beginning with an initial risk evaluation of a hospital’s current practice in VAP prevention to see what documentation procedures were in place to track the occurrences of VAP in the health care setting and in the prevention of VAP, such as tracking hand sanitation, sedation cessation at intervals, periodic weaning evaluations, keeping patients at the required 30 degree head elevation, and periodic tooth brushing. In the evaluation process, the health care staff was required to determine if their present practices were evidence-based, were reported to hospital management, and if there was an established, evidence-based educational program to train staff to prevent VAP.
Once the evaluation had been completed, APIC (2009) recommended a list of procedures and educational materials to maintain trachea tubes to prevent the spread of bacteria, such as the best intubation equipment that was used to minimize the risk of infection, appropriate patient head elevation, and equipment cleaning procedures, the recognition of factors that put some patients at higher risk of developing an infection, and ways collect data consistently to track the implementation of the VAP prevention program.
Reporting was also an essential part of the program according to APIC (2009). Health care facilities established reporting protocols for hospital administrators to track progress, according to APIC (2009). Health care workers were encouraged to keep thorough, detailed records, and used the forms provided by APIC to translate the compliance program’s success into data to track progress in the prevention of VAP within the facility.
The APIC (2009) manual for VAP prevention is included in Appendix A. All procedures, concepts, practice, and training protocols ere described within the manual and served as a source of reference for this study.
Threats to Adherence to Protocol.
As the Agency for Healthcare Research and Quality (n. d.) observed: “No matter how good the bundle that you develop is, if it is not used by the staff it will not be successful” (para. 1). Clarke and Donaldson (n. d.) expressed that factors in the workplace can drastically affect the quality and delivery of care to a patient. Some possible causes of failure to adhere to protocol are understaffing, rate of nurse burnout due to understaffing issues and a stressful environment. Other causes are personal attitudes and lack of cultural cultivation of safety vigilance, a united effort for VAP prevention of best practices within ICU units, a lack of a protocol, and time restrictions (Majid, Foo, & Mokhtar, 2011).
Research Demonstrating Successful VAP Reduction Outcomes Using Ventilator Bundles. Several studies in recent years have proven the effectiveness of ventilator bundling. The studies conducted in an ICU setting all contained many of the features of the APIC system explained above.
The Pennsylvania Patient Safety Advisory (2009) named a few hospitals that were able to bring down their VAP occurrences using ventilator bundles. One of these hospitals was the Roxborough Memorial Hospital (n. d). Before the study, according to the Roxborough Memorial Hospital, the hospital reported steady and increasing numbers of VAP cases for the years 2002 through 2004. After applying a ventilator bundle, they decreased their numbers to only one per year for the following three years, achieving zero cases of VAP in 2007. The success of decreased numbers of VAP cases was due to the implementation of a ventilator bundle protocol.
Some of the factors Roxborough Memorial Hospital (n. d.) that were thought to contribute to the success of the bundle program were teams of healthcare workers from different disciplines worked collectively as a team and provided input into the program implementation and tracking. Moreover, in addition to the preventative measures commonly associated with bundle programs, Roxborough Memorial Hospital reported that keeping, tracking, and analyzing data was pertinent to lowering their numbers for three years.
Korn, Burke, Burke, and Agarwal (2010) reported similar results upon implementation of a VAP prevention program. For their baseline assessment, Korn et al stated their rate of VAP infection was one case of VAP for every 100 hours. After the implementation of the bundle, their occurrences of VAP dropped 60%. “Initiation of a VAP bundle protocol is an effective method for VAP reduction when compliance is maintained” (p.466).
Even when reports on using ventilator bundle to prevent and decrease occurrences of VAP are not as rosy as one would like, one can still look to these studies to find areas of improvement, possible research design flaws, and other matters that might have skewed the results. One such example is a study by Bouadma, Deslandes, Lolom, Le Corre, Mourvillier, Regnier, Porcher, et al. (2010). When they implemented and tested a multifaceted bundle, they almost seemed to be disappointed their results were not close to or at zero cases of VAP for the duration of their research. Cadena, Tierney, and Restrepo (2011) attributed this to missing data in Bouadma’s et al. report. Also, observed Cadena et al., “The authors also included organisms not commonly associated with VAP, such as coagulase-negative Staphylococcus, Enterococcus species, and fungus. Given that microbiological confirmation was required for a VAP diagnosis, these organisms should have been excluded” (p. 1084). In addition, depicted Cadena et al., Bouadma et al. used proton pump inhibitors, which are associated with contributing to the occurrences of VAP. Mistakes like these are valuable lessons for future research designs and other valuable lessons negative or not-as-good-as-anticipated results can bring.
Why VAP Bundles Work.
There are still some doubters who question the effectiveness of VAP bundles, claiming they are oversold as a solution, observed Darves (2005). They cite the reasons for their lack of faith to be that some of the individual practices are not proven as a “stand alone”, evidence-backed measure. However, as Darves pointed out, while some are weakly associated as preventative measures, such as hand washing, one cannot ignore the common sense of the practice, plus when associated with other measures such as head-of-bed elevation, assessment for early weaning, and other practices, the bundles are powerful as a package and have validity as a group. Perhaps it does not even make sense to test each measure in isolation, and it’s unethical, because it would bring the patient harm to use only one measure to improve care rather than use an entire comprehensive system. It makes sense that each measure is weakly associated as stand-alone because strategies starring a single preventative measure could not possibly be as effective as addressing all the possible causes of infection comprehensively.
Conclusions
While each patient arrives with an array of challenges and factors that contributed to their placement within the ICU, there are many factors that are within a nurse’s control that can decrease a health care facility’s incidences of VAP. Where patients are more prone to develop VAP, nurses can still make a significant contribution in decreasing occurrence of VAP even in the most challenging cases, even bringing VAP numbers to zero – “Many hospitals have achieved significant reductions in VAP rates in their critical care units, some even reaching zero by taking a comprehensive and multidisciplinary approach to ventilator care” (Institute for Healthcare Improvement, 2013, para. 1). Having a comprehensive VAP prevention program in place that includes the education of nurses and other staff most closely associated with the patient ‘s care, compliance to safe practice procedures aimed to reduce risk of infection, and meticulous record keeping by staff to keep track of compliance to procedures are essential elements within a comprehensive VAP prevention program. APIC’s program contains all of these elements, and is therefore a good program to use to track results and achieve the goals of this study. Moreover, more validation is needed for these protocols, and the APIC protocol in particular is understudied.
Summary
Chapter 2, the literature review was presented. Hospital-associated causes of VAP were explained, as well as a patient’s inherent characteristics that could increase susceptibility to VAP. Best practices to prevent VAP progressions were described followed by a detailed description of APIC’s VAP prevention protocol, the summary, and conclusion for the chapter.
In chapter 3, the methodology for the study will be introduced and explained. The following elements of chapter 3 will be described in detail: the setting, participants, research design, instrument or research tools, data collection, data analysis, human subjects’ protection, and summary.
Chapter 3: Methodology
Introduction
This chapter contains the methodology for this study. The study setting will be described, as well as the participants. The research design, data collection, and data- analysis will be explained. The measures taken to protect human subjects will be stipulated.
Setting
The setting for this study will occur within an intensive care unit (ICU), where gravely ill patients are most likely to be intubated. The training for the nurses will take place in part in an available room in the hospital. The rest of the training will occur in the ICU. The establishment of the APIC record keeping system will be established throughout appropriate recommended areas throughout the hospital setting.
The Role of the Researcher
According to APIC (2009), a person playing the role of infection preventions’ should be the key person to educate the faculty and be the person to facilitate communication across faculty and hospital administration channels. The researcher will be the person who will garner the participation of any and all hospital staff responsible for the care of the patients. The researcher will be the person to ensure compliance of all staff to protocol, gather relevant documentation, and analyze the results of the study.
Participants
This proposed study is purposed to stress the importance of highlighting VAP guidelines in order to reinforce the preliminary procedures that were put in place to minimize, if not eliminate, the occurrences of ventilator-associated pneumonia (VAP) in the hospital setting. For this proposed study, sixteen nurses work in the ICU setting in this researcher’s hospital and will participate in the study. Since the APIC system suggested guidelines include a systemic support system for the establishment and implementation of a comprehensive infection prevention protocol, the researcher will approach recruitment for the study from the top down. The researcher will seek the approval of the ICU department and the IRB of the hospital to conduct the study within the ICU setting, and obtain permission of all supervisory personnel. Not only will hospital administration have to approve the study, but they will also agree to participate. It is the researcher’s goal to garner as many people as possible from other departments for their expertise in their field and input to form a committee to implement the APIC guidelines. While the numbers of people are not determined at this time, it is the hopes of the researcher to seek out a committee of ten people to include different experts and different members of the hospital administration to stay true to the APIC protocol and benefit from the education and learning collaboration offers, an important part of the study. It is the hopes of the researcher to have every person working in the ICU who has direct contact with ventilator patients to agree to a least participate in the assessment, which would amount to 16 nurses working in the ICU participants in addition to the 16 nurses and any supervisory and administrative personnel relevant to the study and implementation of the APIC .
With the implementation of the APIC protocol, all nurses, regardless of years on the job, training, and ethnicity, will receive identical training on the APIC system of record keeping and procedures for VAP prevention, and should have an equalizing effect upon participant variations that could affect the study’s produced data.
The seriously ill patients also play a part in this study. They suffer from a variety of illnesses that resulted in their stay in the ICU. They come from all walks of life, are various ages, and have a variety of health problems. The one aspect they have in common is they are ill enough to require care in an ICU setting. The inherent factors of the patients discussed in the literature review could produce variations upon the results. However, variations in inherent factors that could leave some patients more vulnerable to infection than others are part of the realistic nature of caring for gravely ill patients, and add to the valuable experiences of this study. As past studies have shown, it is possible to have a year with zero cases of VAP if protocol is followed closely. Therefore, all patients who enter the ICU setting will participate in the study. The number of participating patients is undetermined at this time.
Research Design
A quantitative analysis generates data that can be manipulated (Howell, 2011) to discover if a change in procedures produces a discernible effect upon the occurrences of VAP in an ICU setting. This study will utilize the quantitative framework to discover if the implementation of the APIC protocol will reduce the amount of VAP cases in an ICU setting. A quantitative study will be used for this study to generate hard data that will either prove or disprove the null hypothesis.
Quantitative studies are important for the field of nursing. It produces the data the field needs to decide which practices should be acceptable, which to discard because of ineffectiveness, and which practices to incorporate or supplant older practices because it has been proven they are more effective and have a benefit for the patient. It is the hopes of the researcher that this study will add to the literature and generate the data needed for other hospitals and nursing professionals to make informed decisions based upon valid research.
One might see elements of action research design in this study because of the collaborative nature of APIC VAP prevention bundle. However, because the researcher is leading the study and will perform all calculations and be solely responsible for the generation of the results and subsequent write up of the research, this remains a quantitative research design with community and team learning and education aspects built into the APIC program.
Validity and Reliability
This study was designed with the implementation of the APIC protocol it emphasis on these protocols which show the reliability and validity of this design. The emphasis on these dimensions in this approach was to enhance the study’s validity through a process of survey studies specifically meta-analysis of relevant studies which occurs in those quantitative studies in which validity is achieved through establishing the credibility of the source material, which, in this case, involves the existing research and literature on the subject of ventilator associated pneumonia. This tool will be implementing in the Intensive Care Unit where new nurses in training will be educated. The survey tools leading to credibility within the study involves the integration of existing research that has been subject to peer review and criticism, the unique critical analysis by the researcher, and the inclusion of primary data. This research design is displayed in the figure below:
Description of Instruments or Research Tools
All research tools are provided with the APIC protocol for VAP prevention, which is an evidence-based system of collecting and analyzing data (APIC, 2009). A variety of methods are utilized to gather data – questionnaires, surveys, historical gathering of data from patient files, and reports on observations from participating supervisory hospital staff.
SPSS will be used to generate the dependent t-tests, the normality assumption, and generate the confidence intervals to see if the results of the test are significant. Harvard-MIT Data Centers (n. d.) stated that SPSS is a little limited for complicated analyses. However, for t-tests, it is known as a reliable tool for analysis.
Data Collection
For the baseline assessment, the researcher will garner the historical data from patient records. Each hospital patient’s records, ethnic background, course of illness, and other information pertinent to the APIC protocol and study will be used solely for informational purposes. Each name on the record will be dedacted and replaced with a case number.
The researcher will also seek compliance information from the hospital staff participants. Each participant will be asked to fill out the required paperwork provided in the APIC bundle.
Integrity of Data
The integrity of the data will be maintained on a removable storage device for a desktop or laptop computer. The device will be stored in a locked draw, for which the researcher has the key to ensure safety and integrity of the data.
Data Analysis
A t-test is a method of analysis that is beneficial to use when hardcore data is needed to gauge the effectiveness of implemented protocols. T-tests have validity and are the most widely used analysis (Howell, 2011).
The analysis technique will utilize a dependent t-test. The rationale for the use of the dependent t-test is the experiment will take a preliminary data assessment. The experimental situation, the establishment of the protocol, will be instilled into the practices of the ICU unit. After a predetermined segment of time, the data will be measured at the end. The ending data set will be compared with the first data set. Since there will be a beginning data set, the protocol will be administered, then a collection of data from the same ICU at the end of the experiment, a dependent t-test is desirable to use, according to Howell, to discover if a makes a significant contribution to the reduction of VAP for the month of study. This analysis contrasts independent t-tests, where the origins of the two sets of data are provided from two separate groups, such as a control group and an experimental group, stated Howell. Since this study will look for a change in data from the same setting, a dependent t-test is more appropriate.
The baseline assessment will be performed. Another assessment will be conducted once a month for six months to see if VAP death and acquisition rates have fallen. The data will be tested for normality, and be reported with a confidence interval of 95%.
Other calculations are important to understand the success or failure of the implementation of the APIC bundle. The researcher will be using the APIC (2009) guidelines for conducting a baseline assessment of the ICU unit. A combination of nominal and ordinal data responses are used on the questionnaires for the researcher to complete. The subjects covered are present compliance to VAP protocols (hand washing, sedation vacations/readiness to wean, head-of-bed elevation, and oral brushing/cleaning). The next step is to conduct the assessment. Historical data, the different types of infections and occurrences, must be used to generate meaningful data. After selecting length of time for data examination (which will be one year for this study), financial costs generated from illness and mortality rates per 1000 hours will be generated. The assessment will help generate a supervision plan for the execution of the protocol. Moreover, the baseline assessment data, the death rates, will be used as part of the methodological part of the study as the preliminary data for the dependent t-test.
Human Subjects Protection
Minimizing harm of the participants is built into the research design. This study will be conducted with the permission of the IRB at the hospital. The IRB reviews research proposals and has a set of standards research must meet in order for the study, including the ethical protection of the participants.
In this study, the researcher will take extra measures to protect the participants from harm. Permissions will be sought for nurses’ and other healthcare workers’ participation in the program to ensure they are participating freely. Their will to participate is part of the collaborative environment APIC suggests is created, and will also ensure adherence to protocol, personal responsibility, and free will to participate, minimizing harm. Moreover, the education and training will be applied equally to all hospital staff, so risk of emotional and mental harm will be minimized. Any feedback they provide will be anonymous, so their truthfulness will not produce fear of supervisory discipline.
The study’s entire purpose is to protect the patients from harm, minimizing harm to the patients. Moreover, when patients are signed into the hospital, they or their relatives are informed that the facility is a teaching hospital. Since the study’s purpose is to minimize harm to the patient and improve upon present services using a prevention bundle based upon evidenced-based practice from an authoritative organization dedicated to the prevention of HAPs, harm is minimized to the patient. This in addition to IRB approval will minimize harm to the patient.
Summary
In this chapter, the methodology of the study was explained. The setting, participants and protection of the participants were described. The data analysis, storage, and reliability and validity were explained, as well as the tools used for data collection and calculation was explained. Chapter 4 will explain the findings, if the APIC VAP prevention protocol was effective for reducing VAP incidences and deaths in an ICU setting.
Chapter 4: Findings
Overview Data Analysis
In order to evaluate the information derived from the dataset known as “Epidemiology PMR – FY 2013,” it is important to conduct basis analyses that will evaluate an existing dataset and determine if compliance to the VAP protocol has changed or improved over a period of time, such as one year or four quarters. Based upon the utilization of the dependent t-test for this study, it is important to recognize that this test is basic in nature but provides significant information regarding the validity of a given problem and whether or not the results have changed over time (Howell, 2011). By using patient records that have been generated for a given fiscal year, the statistical significance of the VAP protocol will be determined and quantified. The dataset to be used for the t-test will not include any specific patient identifiers and instead, will include the implementation of the VAP protocol in experimental form in the ICU for data analysis and evaluation.
Quarter 1 – Quarter 2
In comparing the first and second quarter statistics, the following data was derived using a dependent t-test:
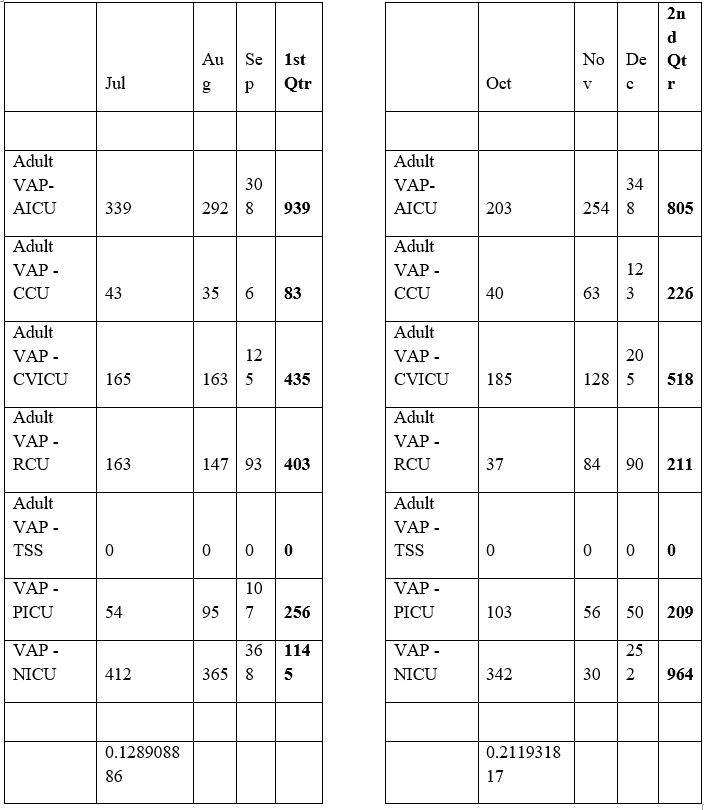
Based upon the results derived from the t-test, the P-value derived from comparing the first and second quarters is 0.128908886, which is deemed statistically insignificant because it is above the commonly used threshold f 0.05. This data demonstrates that in adopting the protocol from the first quarter into the second quarter, there is no statistical difference in compliance rates because the cases of VAP continue to be high overall. Although some areas have declined, such as the AICU, the RCU, the PICU, and the NICU, others have actually increased, such as the CCU and the CVICU. Therefore, the protocol implementation has been met with mixed results from quarter one to quarter two.
In the transition from quarter two to quarter three, the results indicate a P-value of 0.211931817, which remains statistically insignificant. However, this comparison is important because the two quarters demonstrate an increase in VAP cases in all but two units, the RCU and the NICU. All other units experienced an increase in VAP cases, which signifies that the VAP protocol as implemented by nurses has either not been properly utilized and is not well understood, or compliance is poor. The movement from quarter two to quarter three also signifies a potential set of challenges in implementing the VAP protocol over the long term because it has not provided any significant reductions in VAP cases within the majority of the units that were surveyed.
In the transition from quarter three to quarter four, the results indicate a P-value of 0.542958689, which is also statistically insignificant, based upon the threshold for standard P-values:
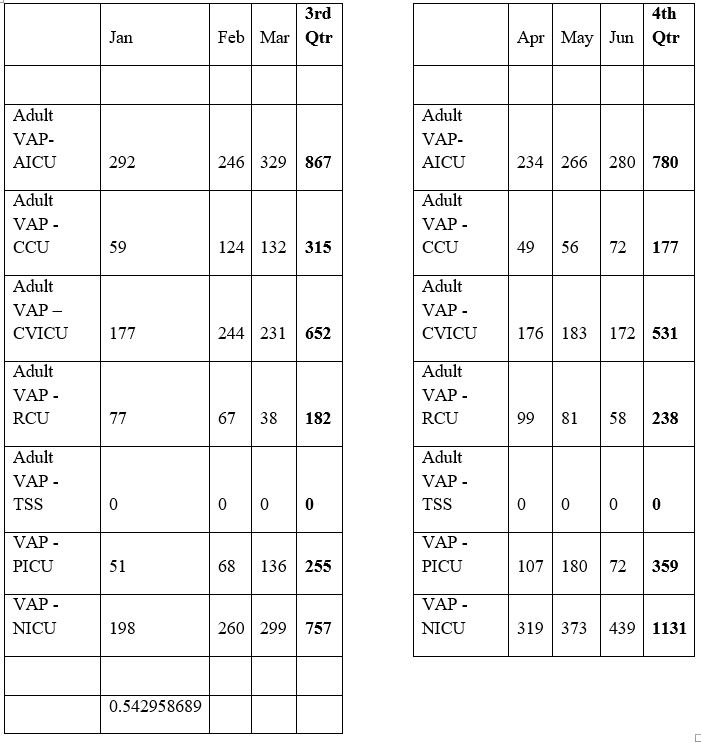
This dataset is somewhat different than the comparison of the prior quarters because there is a general decrease in the number of VAP cases in the AICU, the CCU, and the CVICU. However, there is an increase in cases in the PICU and the NICU, which may demonstrate that there is another circumstance that might have occurred in both of these pediatric units that led to an increased number of VAP cases between these two quarters. This dataset is relevant because it supports the assumption that the method in which the protocol is administered and the training provided to nurses might be different between the adult ICU units and the pediatric ICU units. This is an important assumption because the manner in which pediatric patients are treated is generally different due to the vulnerability of this patient population. Nonetheless, the VAP protocol response and compliance rates appear to be mixed based upon the statistically insignificant results of the t-test alone.
From a researcher’s perspective, the evolution of the VAP protocol must be considered in greater detail because based upon the t-test values; there is little significance and change in the administration of the protocol within the ICU in both pediatric and adult units. Therefore, it is important to recognize that there are other factors at work in this process. It is important to recognize the value of the dataset and that the administration of the protocol appears to be ineffective in reducing overall VAP cases. At the same time, other factors should also be considered, such as the period in which the data was derived, as different months of the year may demonstrate a marked increase in the number of VAP cases, based upon weather and other factors leading to increased illness within a given patient population. Furthermore, other protocols or policies might have been implemented in the different units that nurses must follow, which could have an impact on the ability of this protocol to be successful in reducing VAP cases within these units.
Based upon the data provided and the P-values generated using the dependent t-test method, the hypothesis is null because the data has not demonstrated any real change in the number of VAP cases, in spite of VAP protocol implementation. Although some results are mixed and have increased/decreased on a random basis, this study does not indicate that there is any real benefit to the VAP protocol implementation in its current form in the various ICU units under consideration. In spite of the recommendations provided by the Association for Professionals in Infection Control and Epidemiology (APIC), there is no real benefit to the implementation of this protocol using the case data provided for analysis. However, there is room for interpretation and a possible weak implementation protocol to begin with using the dataset that has been provided.
It is important to identify areas where there are significant challenges in protocol implementation and in determining the protocol’s effectiveness in reducing VAP cases in this group. For example, the results might have been influenced by underlying factors such as poor hand hygiene, which may contribute to poor patient outcomes in the ICU (Pitett, 2003). Furthermore, the tracheal tube might have contributed to the statistics derived during the four-quarter period due to mucus development and limited suctioning (Johns Hopkins Medicine). Other challenges may include poor head elevation, which may contribute to increased cases of pneumonia (Williams, Chan, and Kelly, 2008), in addition to employee-based methods to increase comfort and reduce the risk of VAP within this patient population over a period of time (Maselle, 2011). Each of these factors might have contributed to the variances that were observed in VAP cases across the different ICU units and the statistical insignificance of the VAP protocol for patients.
It is also possible that the study results were distorted as a result of other unknown factors. Nonetheless, the results generally indicate that the implementation protocol has not been successful on a consistent basis in reducing the number of cases of VAP within the ICU setting. The term “inconsistent” is essential to this discussion because it indicates that some nurses might not have implemented the protocol in the desired manner and therefore, led to inconsistencies between quarters. This information is relevant because it supports the need to potentially expand education in regards to the existing protocol or to consider other alternatives to modify the protocol as necessary to support the desired objectives and reduce the number of VAP cases over time. These efforts will demonstrate if the protocol in its current form is effective with additional training, or if the protocol must be modified to better accommodate patient needs.
Perhaps the most significant area to consider with the lack of effectiveness of the current protocol is the lack of understanding of the need for the protocol and whether or not it will make any real difference in patient-related outcomes. Some nurses might perceive that the protocol will not make a difference and is ineffective and therefore, will not fully comply with its requirements. Others may take a different approach and recognize the need for the protocol in spite of the relatively simple risks associated with VAP, yet support its continuation through compliance with the required methods. In either case, nurses who are required to implement the protocol must be on the same page and must demonstrate their commitment to providing optimal patient care in critical care settings, even when there is a risk that the chosen methods will not be effective. Compliance is key in supporting this process and the eventual reduction of VAP cases in ICUs throughout the world.
As a researcher, it is important to identify other obstacles or barriers that might have influenced outcomes and the t-test results. However, it is also possible that environmental factors and general poor or non-compliance with the protocol objectives played a role in these outcomes. It is important to identify the challenges that exist with this protocol and the potential that exists to overcome these challenges and to improve VAP protocol implementation in the future, along with any modifications to the existing protocol as necessary to ensure that greater compliance is achieved and VAP cases are reduced within this patient population. It is important to recognize these conditions because they represent an opportunity to explore the serious nature of VAP and its impact on patient care in ICU settings, particularly when patients possess critical needs and may be in extreme danger, facing death or other complications.
Conclusions
Adherence to protocol requirements, however, may not tell the entire story. Therefore, additional evaluations in other healthcare organizations using the same protocols must also be considered as a feasible alternative to ensure that nurse compliance is maximized and patient care quality is improved through the use of this protocol on a consistent basis. These elements will play an important role in shaping the future directives of ICUs and in supporting the development of new approaches to manage patient outcomes in an effective manner. The implementation of a VAP protocol must continue to be explored for its value and significance in supporting a reduced number of VAP cases and in achieving the desired results within the framework of the ICU patient care setting, as this type of protocol must achieve greater effectiveness within this environment.
Chapter 5: Results and Conclusions
Overview of Research Project
The research project that was conducted provided an investigation of the implementation of a protocol to address the significance of Ventilator-Acquired Pneumonia within the Intensive Care Unit. This protocol was designed by the Association for Professionals in Infection Control and Epidemiology (APIC) in order to reduce the incidence of VAP in ICU patients. This protocol was implemented in a hospital environment with several units, including pediatric, neonatal, and adult intensive care units. Therefore, the protocol implementation was applied across the organization to ensure consistency in executing the selected APIC protocol. The study analyzed the data observed regarding the incidence of VAP cases in quarterly intervals for up to one year after protocol implementation. In addition, a questionnaire was distributed to nurse participants in order to determine if the protocol was effective and if it achieved the desired purpose within the ICU framework.
Summary of Findings
The research study sought to implement a protocol that could potentially reduce the incidence of VAP in patients requiring mechanical ventilation. This protocol represented an opportunity for nurses to adhere to a specific set of requirements and to demonstrate their knowledge, understanding, and level of compliance with the chosen protocol. Based upon the implementation of the protocol, it was determined that from one quarter to the next, there were inconsistencies in the number of VAP cases per unit, with some units experiencing increases and others experiencing decreases. This demonstrated that in its current state, the VAP protocol was ineffective in providing the desired reduction of VAP diagnoses across the different units on a quarterly basis. These findings suggest that there are significant factors associated with the implementation of a given protocol within a patient care setting that may be influenced by environmental conditions or other forces, such as low compliance with every aspect of the chosen protocol.
How Results were Obtained
The results were derived by using a data collection process in order to identify the frequency of VAP cases within the different ICU units at the selected hospital. The data collection was derived from case records and was recorded on a quarterly basis in order to determine if there were any patterns or changes to the number of VAP cases across the different ICUs. This information was useful because it provided greater insight into the effectiveness of the VAP protocol and whether or not it could have a significant impact on the outcomes of patients who are dependent on mechanical ventilation. Under these conditions, if the protocol was effective, there would be a marked decrease in the incidence of VAP cases across the different ICUs that were evaluated. If the protocol was not deemed effective, then it would not have a significant impact on reducing the number of VAP cases within the ICUs. The data collection method was necessary in order to capture an understanding of the number of VAP cases and why there is a continuous risk of VAP for patients who require mechanical ventilation. An effective protocol is necessary to reduce the number of cases and to promote nurse effectiveness in adhering to the protocol guidelines. This provides an opportunity to explore the different dimensions of a protocol and to determine if it will be effective in achieving its stated objectives in a successful manner.
Solutions to the Research Problem
The research problem in question is challenging and complex for many reasons. Therefore, it is necessary to identify possible solutions that will have a favorable impact on patient outcomes and on the ability of nurses to achieve maximum compliance with the protocols that they are given. These practices will ensure that nurses are able to understand the protocol and adhere to its requirements at all times. However, the protocol must be appropriate for the given population and must address as many areas as possible that will enhance the quality of care and reduce the risk of infection for this patient population. Due to the precarious health of these patients and their weakened immunity, all possible measures must be taken in order to achieve effective outcomes. Therefore, in the absence of an effective protocol as demonstrated in the research study, other possibilities must be explored, which may include this protocol along with other guidelines or a combination thereof.
Implications and Limitations
This research study provided an important step towards the discovery of new concepts in order to implement protocols that might be effective in reducing the incidence of VAP in patients. It is important to identify areas where VAP infections are likely to occur and to determine the types of patients that might be affected by this condition within their lives. This study has significant implications for the area of VAP research because additional protocols must be considered that may have a greater impact on patient outcomes. These elements are critical because they contribute to the effectiveness of a given VAP protocol and the success rate that it provides in the form of reduced numbers of VAP cases. Based upon the information provided in this VAP protocol, additional measures must be considered in other protocol forms in order to accomplish the desired objectives and to provide patients with a minimal risk of infection. This is an important step towards the discovery of new techniques and strategies to accommodate patients who require mechanical ventilation so that their recoveries are not compromised in any way during their time in the ICU.
Strengths
The research study provided a strong basis for evaluating a VAP protocol upon its implementation in a number of ICUs. The use of a single facility with several different types of ICUs that serve a number of populations from neonates to adults represents an opportunity to utilize the protocol in a number of different patient care environments.
Weaknesses
It is important to recognize the value of the VAP protocol as a means of establishing benchmarks for nursing compliance in order to determine if additional frameworks or protocols must be identified. In this instance, it is necessary to expand the protocol to other sites in order to determine if the problems are related to that specific organization or if the protocol is weak to stand on its own. These elements pose a challenge to the integrity of the protocol and its potential impact on the ability to reduce VAP-related infections in ICU patients who require mechanical ventilation.
Problems Noted with the Project
The protocol implementation in the research study was relatively smooth; however, based upon the study results, it is necessary to expand the protocol to a larger population in order to determine its effectiveness in meeting the desired outcomes. In this context, the study was limiting, but did not pose any real problems for the researcher or the organization as a whole.
Factors that Skewed Findings
The limiting nature of the study in a single facility was challenging for the researcher and might have played a role in the limited results that were derived. It was important for the researcher to conduct the study in a single facility to gauge its probability for success in a larger number of facilities. Nonetheless, the study was not entirely successful in its approach or its scope. Furthermore, the possibility of external environmental factors played a role in the outcomes of the study and its limited impact on VAP infections. Therefore, the findings of this study were not as comprehensive and as effective as anticipated.
How Study Could be Improved
The study could be improved in a number of ways, including a more precise evaluation of nursing compliance with the VAP protocol. In addition, an expansion of the study to additional sites may have an impact on the study results that are derived in the future. This may also have an impact on long-term outcomes for patients who are at risk of VAP in ICU settings.
Areas for Further Investigation
It is expected that patients in the ICU will be most impacted by this study. However, nurse perspectives, knowledge, and education must also play a role in shaping these outcomes in future studies. The retention of nursing knowledge is critical to this process. It also supports the development of an approach that will aim to reduce VAP infections in ventilator-assisted patients in the ICU.
What to do Differently in the Future
For future variations of this study, it is important to attempt to overcome any possible issues regarding compliance that are likely to occur with this study. If the same protocol is implemented elsewhere, lessons should be learned that will accommodate the needs of ICU patients in other settings.
Justification of Differences
It is also important to modify the study as necessary to ensure that future outcomes are successful. This may include the development of new additions to the existing protocol in order to achieve improvements in the form of reduced VAP cases.
Reflection on Master’s Degree Experience
This experience has been highly beneficial in demonstrating the importance of new perspectives regarding research and its impact on nursing practice. Prior to this experience, I did not have a full awareness of the importance of evidence-based practice objectives and their influence on patient outcomes. However, I now recognize that this process is instrumental in shaping outcomes for patients and in enhancing the quality of nursing care and treatment as derived from existing practice models. These contributions will play a critical role in supporting positive patient outcomes through the reduced risk of VAP infections. However, this model also represents a larger framework that captures the essence of patient care needs, particularly in critical care settings. These elements are critical to the Master’s Degree experience because they support student engagement and learning regarding an unfamiliar research area.
How Skills and Experience may Apply to Work Environment
This skill set and level of experience is useful because it enables nurses to acquire valuable experience in the research field from which the results may be applicable to patient care settings. These elements play an important role in the creation of a learning environment that extends beyond the classroom setting. Therefore, these skills and experiences are essential contributors to the achievement of successful patient care outcomes and the delivery of high quality care and treatment at all times. Evidence-based practice objectives as supported by the research protocol will have a lasting impact on patient care and treatment and will demonstrate the importance of new directions and approaches to encourage patient care that is conducive to greater health and wellbeing throughout the life span. This experience is critical to these objectives and in sustaining the growth of patient care objectives throughout all areas of nursing practice.
References
Agency for Healthcare Research and Quality (n. d.). How do we implement best practices in our organization? U. S. Department of Health and Human Services. Retrieved from http://www.ahrq.gov/professionals/systems/long-term-care/resources/pressure-ulcers/pressureulcertoolkit/putool4.html
Amanullah, S. (2013). Ventilator-Associated Pneumonia Overview of Nosocomial Pneumonias. Medscape Reference: Drugs, Diseases, and Procedures. Retrieved from http://emedicine.medscape.com/article/304836-overview
Amin, A. (2009). Clinical and economic consequences of ventilator-associated pneumonia. Clin Infect Dis., 49(Supplement 1), S36-S43. doi: 10.1086/599814
Association for Professionals in Infection Control and Epidemiology (APIC). (n. d.). About APIC. Retrieved from http://apic.org/About-APIC/About-APIC-Overview
Association for Professionals in Infection Control and Epidemiology (APIC). (n. d.). About APIC: Public policy and advocacy. http://apic.org/Advocacy/Government-Affairs-and-Advocacy
Association for Professionals in Infection Control and Epidemiology (APIC) (2009). Guide to the Elimination of Ventilator-Associated Pneumonia. Retrieved from http://www.apic.org/Resource_/EliminationGuideForm/18e326ad-b484-471c- Bangert-Drowns, R.L. (1986). Review of developments in meta-analytic method. Psychological Bulletin 99 (3), 388-399.
Bird et al. (2010). Adherence to ventilator-associated pneumonia bundle and incidence of ventilator-associated pneumonia in the surgical intensive care unit. Arch Surg. 145(5), 465-470.
9c35-6822a53ee4a2/File/VAP_09.pdf
Bouadma, L., Deslandes, E, Lolom, I, Le Corre, B., Mourvillier, B., Regnier, B., Porcher, R., et al. (2010). Long-term impact of a multifaceted prevention program on ventilator-associated pneumonia in a medical intensive care unit. Clin Infect Dis., 51, 1115–1122. PMID: 20936973
Cadena, J. Tierney, C. J., & Restrepo, M. I. (2011). Preventing ventilator associated pneumonia: Looking beyond the bundles. Clin. Infect. Dis., 52(8), 1083-1084.
Cohen, L., Manion, L., & Morrison, K. R. B. (2007). Research Methods in Education. Routledge: London.
Center for Disease Control and Prevention (CDC). (2012). Healthcare-associated infections (HAI): Ventilator-associated pneumonia. Retrieved from http://www.cdc.gov/hai/vap/vap.html
Clarke, S. P., & Donaldson, N. E. (n. d.). Nurse staffing patient care quality and safety. In Patient Safety and Quality: An Evidence-Based Handbook for Nurses, 1-25. Retrieved from http://www.ahrq.gov/professionals/clinicians-providers/resources/nursing/resources/nurseshdbk/ClarkeS_S.pdf
Critical Care Nurse Training Standards Task Group (n. d.). Final report: Critical Care – Secretariat. Retrieved from http://www.caccn.ca/en/files/mohltc_report_ccn_stds.pdf
Darves, B. (2005). Seven strategies to prevent VAP: a look at the evidence. Today’s Hospitalist. Retrieved from http://www.todayshospitalist.com/?b=articles_read&cnt=262
Devo, P. (n. d.) Pathway to excellence: Are you ready to apply? Retrieved from http://www.nursecredentialing.org/Pathway/PathwayResources/Pathway-AssessmentGapAnalysis.pdf
Harvard-MIT Data Centers. (n. d.). Guide to SPSS. Retrieved from http://www.hmdc.harvard.edu/projects/SPSS_Tutorial/spsstut.shtml
Howell, D. C. (2011). Fundamental statistics for the behavioral sciences. Belmont, CA: Wadsworth Cengage Learning.
Institute for Healthcare Improvement. (n. d.) Ventilator-associated pneumonia. Retrieved from http://www.ihi.org/explore/VAP/Pages/default.aspx
John Hopkins Medicine (n. d.). Suctioning. Retrieved from http://www.hopkinsmedicine.org/tracheostomy/living/suctioning.html
Kempnich, J. (2011). Utilizing decision acceleration for Magnet® gap analysis. Nursing Management, (42)2, 43–45. doi: 10.1097/01.NUMA.0000393001.11257.a5
Kollef, M. H. et al. (2008). Silver-coated endotracheal tubes and incidence of ventilator-associated pneumonia: the NASCENT randomized trial. JAMA 300, 805-813.
Koenig, S. M. & Truwit, J. D. (2006). Ventilator-Associated Pneumonia: Diagnosis, Treatment, and Prevention. Clinical Microbiology Reviews, 19(4), 637-657. doi: 10.1128/CMR.00051-05
Korn, C., Burke, R., Burke, P., & Agarwal, S. (2010). Adherence to ventilator-associated pneumonia bundle and incidence of ventilator-associated pneumonia in the surgical intensive care unit. Arch Surg., 145(5),:465-470.
Lacherade, J. C. et al. (2011). Intermittent subglottic secretion drainage and ventilator-associated pneumonia: a multicenter trial. Am J Respir Crit Care Med 182, 910-917.
Lau, G., O’Keefe-McCarthy, S., & Santiago, C. (2008). Ventilator-associated pneumonia bundled strategies: an evidence-based practice. Worldviews Evidence Based Nursing. 5(4):193-204. doi: 10.1111/j.1741-6787.2008.00140.x.
Majid, S., Foo, S., & Mokhtar, I. A. (2011). Adopting evidence-based practice in clinical decision making: nurses’ perceptions, knowledge, and barriers. Journal of the Medical Library Association, 99(3), 229-236.
Maselle, D. J. (2011). Therapeutic Advances in Respiratory Disease Strategies in the Prevention of Ventilator-associated Pneumonia. Ther Adv Resp Dis. 5(2):131-141. Retrieved from http://www.medscape.com/viewarticle/739619
McAuley, L., & Ramsay, C. (2002). Cochrane Effective Practice and Organisation of Care Review Group (EPOC): Data Collection Checklist. Retrieved from http://epoc.cochrane.org/sites/epoc.cochrane.org/files/uploads/datacollectionchecklist.pdf
Miller, M. A. et al. (2011). A polyurethane cuffed endotracheal tube is associated with decreased rates of ventilator-associated pneumonia. J Crit Care 26, 280-286.
Morris, A. C. et al. (2011). Reducing ventilator-associated pneumonia in intensive care: Impact of implementing a care bundle. Crit Care Med 39, 2218-2224.
Nseir, S., et al. (2011). Continuous control of tracheal cuff pressure and micro-aspiration of gastric contents in critically ill patients. Am J Respir Crit Care Med 184, 1041-1047.
Paciella, M. E. (2009). “Bundle” up to prevent pressure ulcers. American Nurses Today, 4(4). Retrieved from http://www.americannursetoday.com/article.aspx?id=5886
Pennsylvania Patient Safety Advisory. (2009). Successful Reduction of Ventilator-Associated Pneumonia. Pa Patient Saf Advis, 6(2):63-8.
Pipe, T. B., Wellik, K. E., Buchda, V. L., Hansen, C. M., & Martyn, D. R. (2005). Implementing evidence-based nursing practice. Urol Nurs., 25(5),365-370.
Pittet, D. (2003). Hand hygiene: improved standards and practice for hospital care. Current Opinion in Infectious Diseases, 16, 327–335. Retrieved from http://www.intelligentm.com/articles/ArticleImprovedStandardsPractice.pdf
Roxborough Memorial Hospital. (n. d.). Ventilator-associated pneumonia trends, 2002-2008. Retrieved from http://patientsafetyauthority.org/ADVISORIES/AdvisoryLibrary/2009/Jun6%282%29/PublishingImages/66_fig1.JPG
Siempos, I. I., Ntaidou, T. K., & Falagas, M. E. (2010). Impact of the administration of probiotics on the incidence of ventilator-associated pneumonia: a meta-analysis of randomized controlled trials. Critical Care Med 38, 954-962.
Tablan, O. C., Anderson, L. J., Besser, R., Bridges, C., & Hajjeh, R. (2004). Guidelines for preventing health-care-associated pneumonia, 2003. Center for Disease Control and Prevention (CDC), 52(RR03), 1-36. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5303a1.htm.
Terragni, P. P.et al. (2010). Early vs. late tracheotomy for prevention of pneumonia in mechanically ventilated adult ICU patients: a randomized controlled trial. JAMA 303, 1483-1489.
Wip, C., & Napolitano, L. (2009). Bundles to prevent ventilator-associated pneumonia: how valuable are they? Current Opinion in Infectious Diseases 22, 159-166
Vanderbilt University Medical Center (n. d.). Nursing quality and performance improvement plan. Retrieved from http://www.mc.vanderbilt.edu/documents/Magnet%20Website/files/Nursing%20Quality%20Plan.pdf
Vima Medical (2011). HOB Alert: VAP Background. Retrieved from http://www.hobalert.com/vap_bg.html
Williams, Z., Chan, R., & Kelly, E. (2008). A Simple device to increase rates of compliance in maintaining 30-degree head-of-bed elevation in ventilated patients. Critical Care Medicine, 36(4), 1155-1157. Retrieved from http://www.medscape.com/viewarticle/574911

Time is precious
don’t waste it!

Plagiarism-free
guarantee

Privacy
guarantee

Secure
checkout

Money back
guarantee






